#SimBlog: Peter Palpitation
““Peter is a 14-year-old boy who presented to the ED with sudden onset palpitations whilst getting dressed for school this morning. He feels lightheaded and dizzy.””
Observations
A – Patent, talking
B – RR30, Sats 99% in air
C – HR240, CRT 2 seconds, BP 120/80
D – GCS 15/15, BM 5
E – Temp 37.3°C
Clinical findings
Radial pulse felt, too fast to count
No signs of shock
No signs of intercurrent infection
Why we simulated?
Supraventricular tachycardia (SVT) is the most common arrhythmia seen in children. The term can be used to describe any tachycardia originating above the level of the Bundle of His (the fibres passing from the Atriventricular Node (AVN) to the interventricular septum. These tachycardias arise in most cases from cardiac tissue with abnormal automaticity or via a re-entrant mechanism. Predisposing factors include electrolyte imbalances, thyrotoxicosis and myocarditis.
Re-entrant SVTs are caused by an accessory pathway, either within the AVN or between the atria and ventricles at another site, allowing for uncontrolled and repeated stimulation of ventricular contraction.
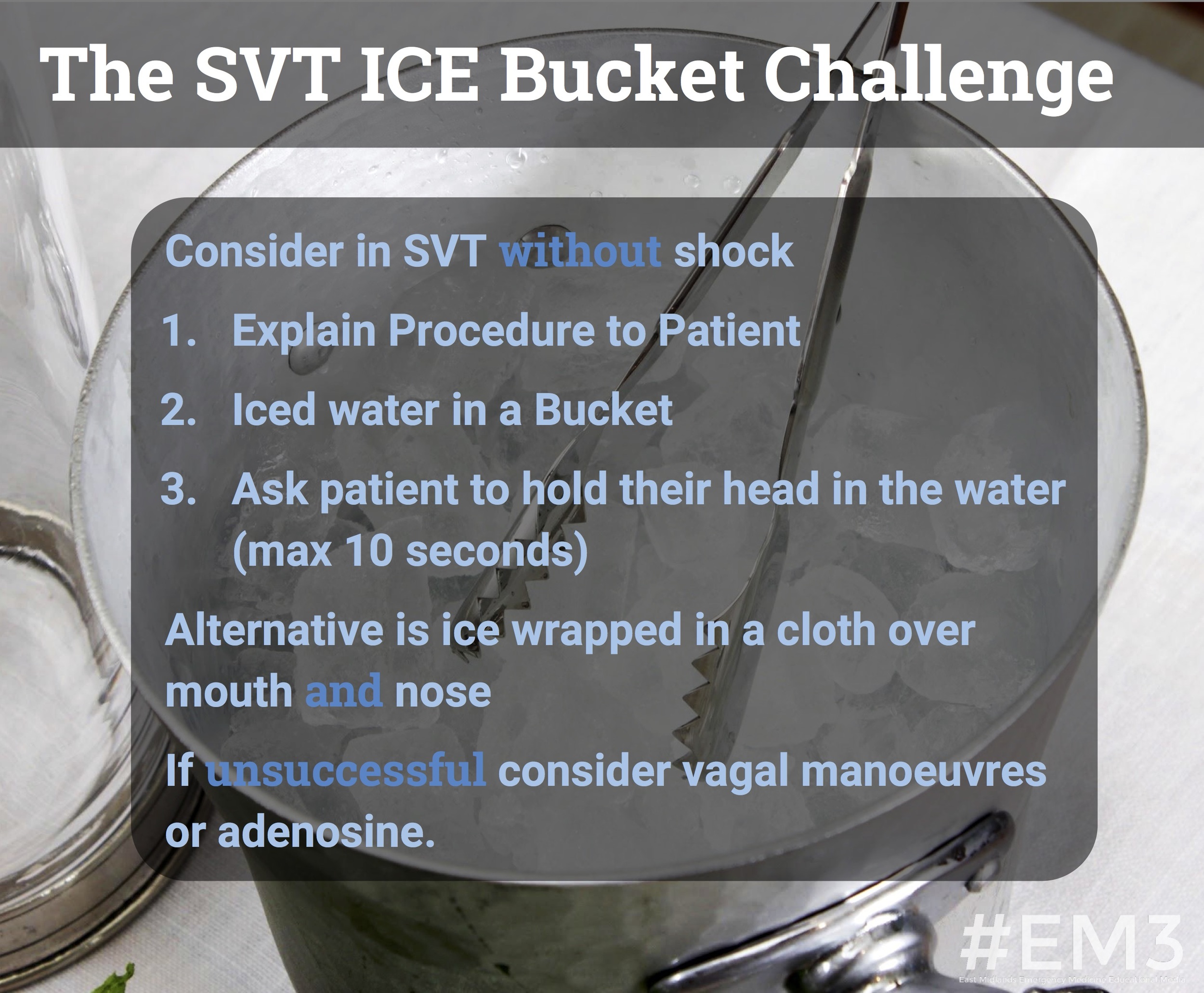
Older children with SVT typically present with episodes of palpitations, chest pain and dizziness. Babies may present in extremis with signs of heart failure, following prolonged episodes of SVT which have not been detected. Initial management of a tachycardia involves making an A to E assessment, looking for signs of shock and infection and performing an ECG to identify the underlying arrhythmia. If SVT is identified, further treatment required in the ED involves a trial of vagal manoeuvres followed by a rapid bolus of IV adenosine or synchronous DC shock, depending upon the clinical status of the child.
We performed this simulation to ensure the team had a good understanding of this initial assessment and management, whilst also being able to source the equipment they needed and explain vagal manoeuvres and adenosine administration to the child and their parent.
Further Reading:
- Life in the Fast Lane: Supraventricular Tachycardia
- APLS: SVT Management
- #EM3: Our Previous (Adult) SVT SIMBLOG and Links to the Revert Trial
Learning outcomes
Try vagal manoeuvres first in a child with SVT with no signs of shock.
Adenosine should be given rapidly through a cannula sited in a proximal vein with a large saline flush.
Communicating clearly with your colleagues and sharing ideas brings together a structured team approach.
Positive feedback
Initiated high flow oxygen rapidly.
Good communication with simulated patient, providing appropriate explanations of how to perform vagal manoeuvres.
Demonstrated awareness of the paediatric SVT algorithm.