Resus Drills: Caesarean Section
Drill pre-brief (instructor to read out)
“Welcome to this Resus Drill. Drills are for situations which are not common, and need a time-critical response. This is not a Simulation. Drills are a rehearsal for practising teamwork and speed.
We will run a scenario for 5 minutes, chat and reflect on it, then run the same scenario again for another 5 minutes.”
Assurances
Learning, NOT assessment: drills are for practice and for learning. We’re concentrating on how fast you can think, and how well you work as a team.
Safe zone: lessons are shared here, not judged, not told as tales.
5-min reflection rules: please use the debrief to be positive about what you can all do better on the re-run. These are deliberately tough scenarios. That’s the point of a drill.
Pretend it’s real: although it’s not real, we need you to help us by acting as you’d do in real life, in your normal role, and we’ll try to run it in real time.
Take-away pack: there is some information that you can take away for further learning. We recommend “spaced repetition” for the best learning!
Make some reflective notes while it’s fresh in your mind
Make yourself read them again in a couple of weeks
How does it work?
Each Resus Drill pack follows a standard format.
The drill packs are laminated and available for teaching purposes. Printable copies can be downloaded HERE.
Our drills can also be EDITED to suit your local hospital needs (Google account required).
S.E.T.U.P. (before patient arrives)
SELF… physical readiness (stay calm) & cognitive readiness (accept the challenge)
ENVIRONMENT… lighting, crowd control, appropriate equipment?
TEAM… initial briefing, identify Team Leader, allocate team roles
UPDATE… if possible, recap for the team (and yourself) before patient’s arrival
PATIENT… the patient arrives
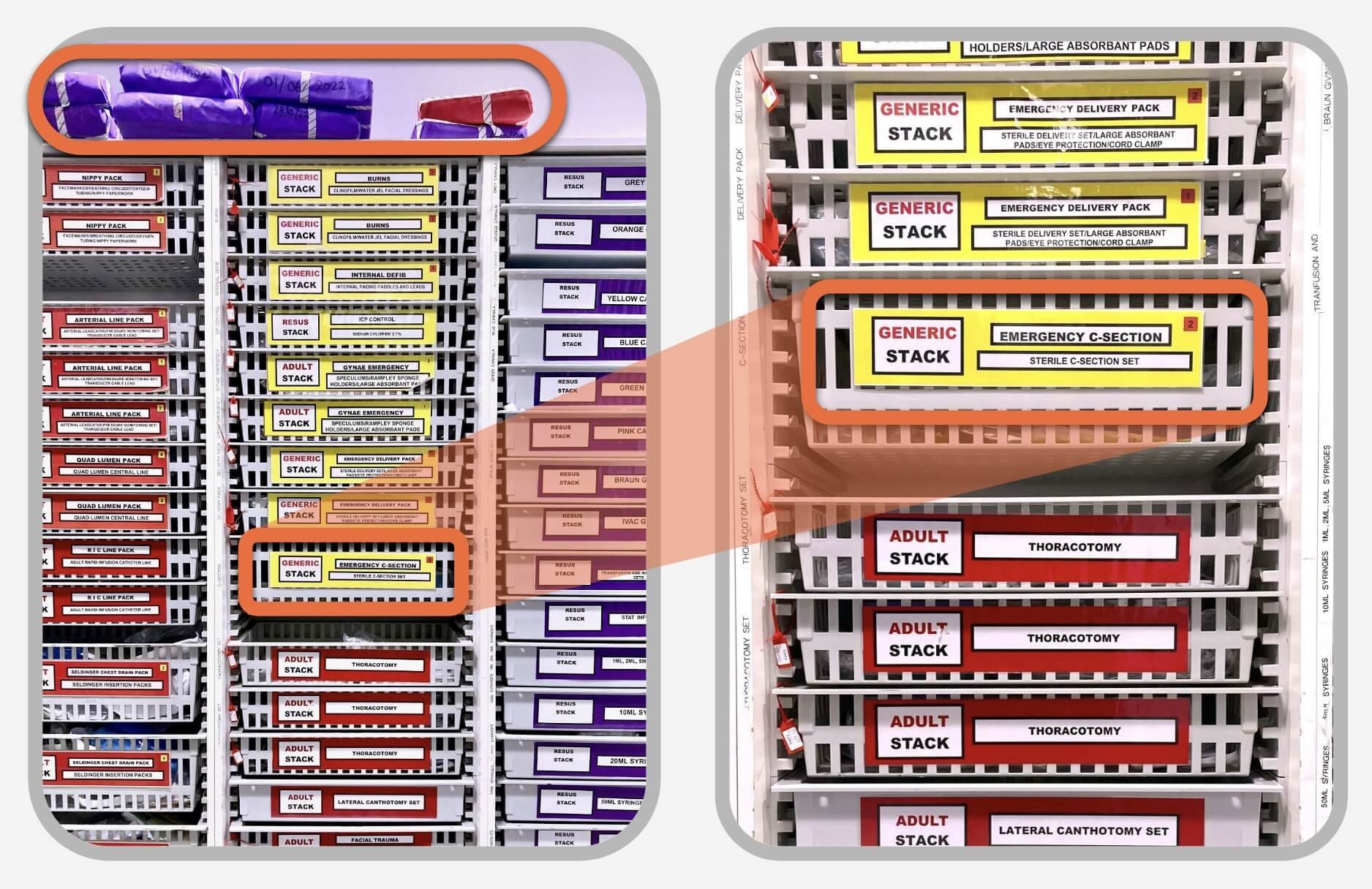
Location of Equipment
A simplified C-section kit should be located in the Resus/Emergency Room equipment stacks and ready to go. A full obstetric pack is not immediately required, but should be nearby when needed (shown on top shelf).
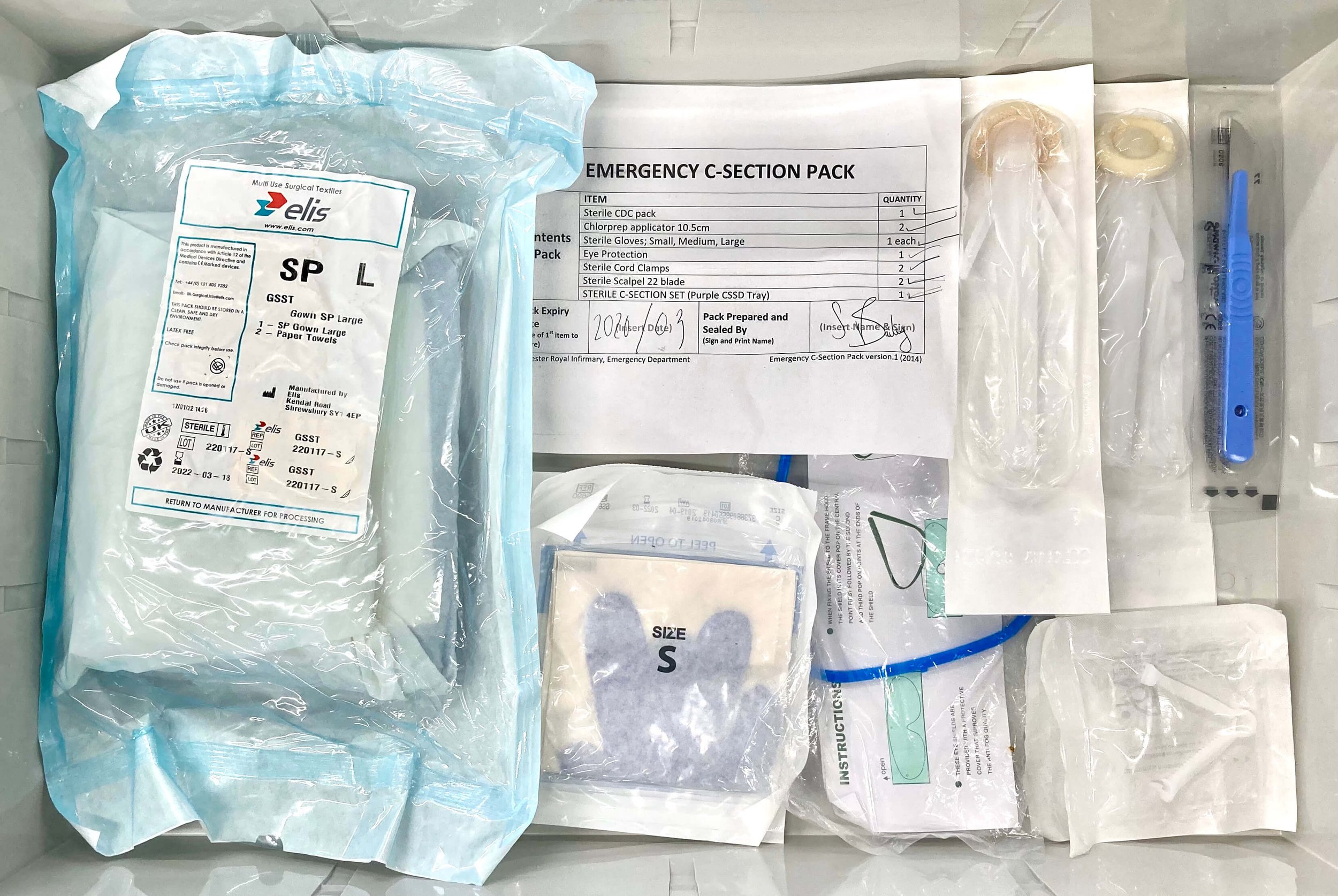
Here are the contents of a simplified C-section kit that will be needed for this drill.
Syntometrine should also be easily found in a nearby Emergency Room refrigerator.
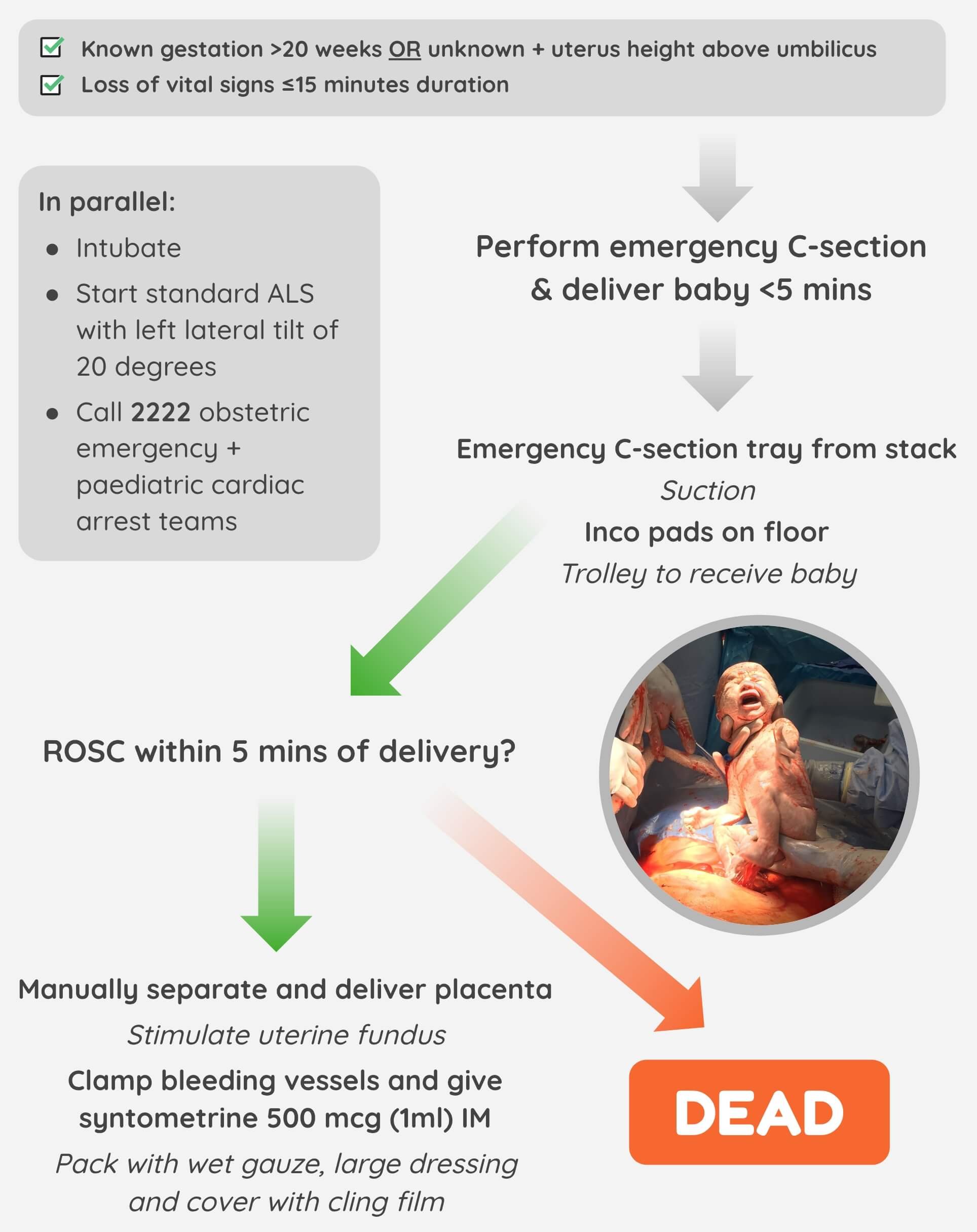
Indications
MATERNAL CARDIAC ARREST + NO RESPONSE TO CPR and left lateral position after 2 MINUTES + gestational age >20 weeks (fundus at or above umbilicus).
Equipment Required
Scalpel
Cord clamp (x2)
Suction
Celox gauze
Large dressings
Cling film
Landmarks and Techniques
Step 1: Vertical incision: xiphisternum to pubis
Step 2: Continue down through abdominal wall and peritoneum
Step 3: Push bowel out of the way
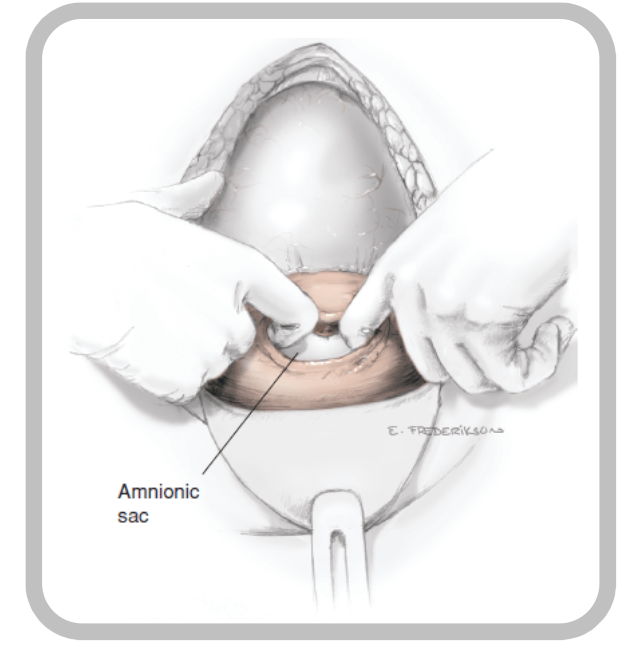
Step 4: 4 cm vertical incision high up the uterus
Step 5: Blunt extension of incision using fingers
Step 6: Deliver foetus (grab any part)
Step 7: Clamp and cut umbilical cord, stimulate with warm towel
Step 8: Remove placenta and membranes, rub uterus
Step 9: Give Syntometrine I.M.
Step 10: Pack abdomen with Celox gauze and dressing, wrap with cling film
Cardiac Arrest Decision Algorithm
Red Call Sheet
Scenario Script
“You have received a 3-minute warning of a 28-year-old female who had onset of severe shortness of breath 1 hour ago, and has a past medical history of PE. She is 35 weeks pregnant. Here is the Red Call form.” (give to Team Leader)
Minute One
Team Leader designates team members and uses S.E.T.U.P. (Self, Environment, Team, Update, Patient arrives). Maintain this phase as real-time as possible. Team Leader should at least consider ITU support and the obstetric emergency team at this stage. Team needs to get the C-section pack (not normal delivery pack) from the ER stacks. Do not prompt if incorrect.
Minute Two
Your patient has arrived. She has a poor colour, is gasping, and not very responsive. So far the ambulance crew have established IV access and started a 500ml bag of saline). Team should measure all obs, obtain 2nd IV access, O2 high-flow. Obs are as pre-hospital red call sheet. Patient is unable to answer questions, gasping.
Minute Three
“She has just gone floppy, pale and her eyes have rolled up.” Cardiac monitor should show SR (it is PEA). Pulse should be checked. Prompt if necessary. “There is no pulse.” Team Leader should initiate lateral tilt, CPR and airway control. Do not prompt tilt maneuver.
Minute Four
“She remains in PEA arrest”. Team Leader should make decision to do C-section (self or other senior Dr), and call for either Paeds ED staff or paediatric arrest call for baby, plus senior support (ED consultant). If C-section started, ask Team Leader to talk through the technique. If reaching Minute Five, cover this briefly in the debrief instead.
Minute Five
“The paeds team, obstetric team and ED consultant have arrived”. Team Leader should manage ‘crowd control’ and noise (ideally by tasking ED consultant with scene management).
Debrief and Feedback
You should aim to cover the following points within 5 minutes, then re-run the scenario:
Did the Team Leader allocate roles and tasks in a way that was clearly understood? Was S.E.T.U.P utilised?
Did the team make the right emergency calls (obstetric emergency team, paediatrics / paeds ED team, anaesthetist and ED consultant?
Did the Team Leader rapidly reach a decision to proceed to C-section?
Did the Team Leader explain the situation in a way that everyone understood it was a time-critical operative procedure?
Did the Team Leader ask for the right equipment and was it provided?
Was the right action taken, to deal with the baby? (PED team or paed arrest call, either appropriate)
Did the Team Leader display knowledge of the technical skills required?
How did team members help the team pull together?
Were there any instances of:
Equipment issues?
Human factors negatively impacting communication or patient care?
Additional Resources
- Procedural Aide Memoires – PAMs: Peri-mortem Caesarean (MAGPAS)
- Prehospital resuscitative hysterotomy: Perimortem Caesarean Section (R.Parry, et al.)
- Post-Mortem C-Section: A How-to Guide to Section or Not to Section (BroomeDocs)
- Prehospital resuscitative hysterotomy (R.Bloomer, et al.)
- Perimortem Caesarean section (LITFL)
- Maternal Collapse in Pregnancy and the Puerperium guideline (RCOG)
- Perimortem C-section (St. Emlyn's)
- Out-of-hospital perimortem cesarean section (D.Kupas, et al.)
- Resuscitative Hysterotomy 101 (SMACC)
- Realistic simulation by obstetricians (Operative Experiences)
- Real-time simulation scenario of a perimortem caesarean section (BTHFT)
- Perimortem C-section simulation (The Gurney Room)