Resus Drills: Unexpected Delivery
Drill pre-brief (instructor to read out)
“Welcome to this Resus Drill. Drills are for situations which are not common, and need a time-critical response. This is not a Simulation. Drills are a rehearsal for practising teamwork and speed.
We will run a scenario for 5 minutes, chat and reflect on it, then run the same scenario again for another 5 minutes.”
Assurances
Learning, NOT assessment: drills are for practice and for learning. We’re concentrating on how fast you can think, and how well you work as a team.
Safe zone: lessons are shared here, not judged, not told as tales.
5-min reflection rules: please use the debrief to be positive about what you can all do better on the re-run. These are deliberately tough scenarios. That’s the point of a drill.
Pretend it’s real: although it’s not real, we need you to help us by acting as you’d do in real life, in your normal role, and we’ll try to run it in real time.
Take-away pack: there is some information that you can take away for further learning. We recommend “spaced repetition” for the best learning!
Make some reflective notes while it’s fresh in your mind
Make yourself read them again in a couple of weeks
How does it work?
Each Resus Drill pack follows a standard format.
The drill packs are laminated and available for teaching purposes. Printable copies can be downloaded HERE.
Our drills can also be EDITED to suit your local hospital needs (Google account required).
S.E.T.U.P. (before patient arrives)
SELF… physical readiness (stay calm) & cognitive readiness (accept the challenge)
ENVIRONMENT… lighting, crowd control, appropriate equipment?
TEAM… initial briefing, identify Team Leader, allocate team roles
UPDATE… if possible, recap for the team (and yourself) before patient’s arrival
PATIENT… the patient arrives
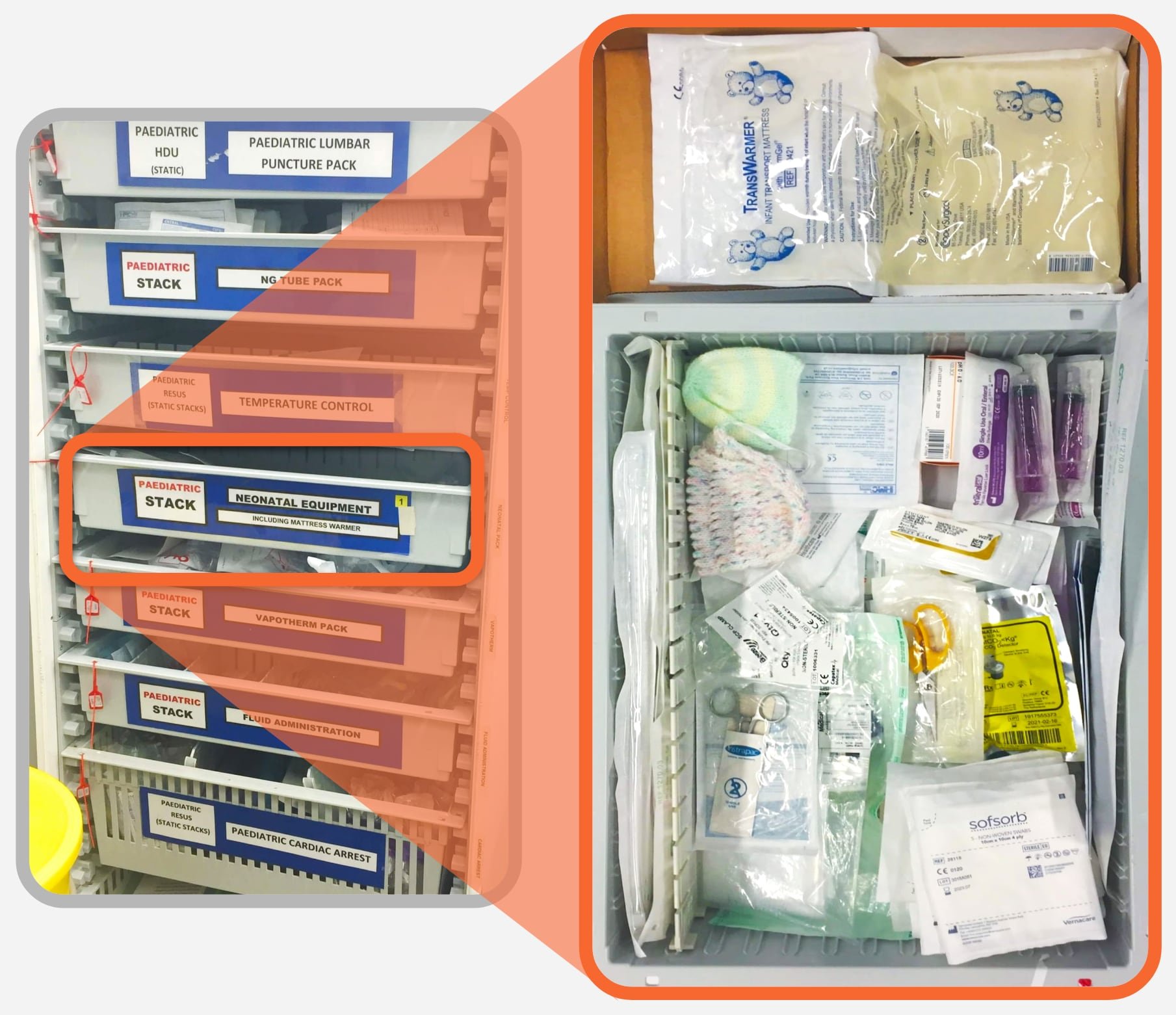
Location of Equipment
An Emergency Delivery Pack should be available in your Resus/Emergency Room equipment stacks. Here’s a look inside…
Other useful Neonatal Equipment required post-delivery should also be prepared. The contents may contain a TransWarmer heating pad, cord clamps and a hat for baby.
Equipment Required
Essentials: Towels, Emergency Delivery pack (kit needed for mum), Neonatal Equipment stack (kit needed for baby)
Emergency Delivery pack
Sterile CDC pack
Sterile delivery pack
Chloraprap applicator 10.5 cm
Sterile gloves (Small, Medium, Large)
Sterile gown
Eye protection
Sterile cord clamps
Large absorbent pads
Neonatal Equipment pack
Umbilical Catheters (size 3.5 Fr & 5 Fr)
Gauze (10x10 cm)
Silk sutures (2.0) + Steristrips
Sterile scissors
Stitch cutter
Nylon cord
Air Flow & Oxygen Low flow meter
Neopuff resuscitation system
Landmarks and Techniques
Step 1: Cord clamping
Place one clamp approximately 15 cm from the baby’s abdomen
A second clamp 2–3 cm distally to the first
Ensure that they are firmly closed and cut between
Step 2: Basic neonatal resuscitation
Dry and rub (stimulate) with warm towels and check response and heart rate (should be >60/min)
BLS highly unlikely to be needed, wrap baby in dry, warm towels and keep separate from mum for now (until mum assessed and facts established)
Apply TransWarmer under wrapped baby and a hat
Step 3: 3rd stage of labour
Support the mother in a comfortable position…
Upright at 45° if no bleeding, never flat
Passively assist the mother, do not pull the cord…
Expulsion of placenta + membranes can take >15-20 mins
Deliver straight into a bowl or plastic bag and keep
Once placenta is delivered (end of 3rd stage)…
Massage lower abdomen with a cupped hand using a circular motion to stimulate uterine contraction
Administer Syntometrine I.M. (kept in ER fridge)
Unexpected Premature Delivery Decision Algorithm
Scenario Script
“An alarm is set off from the Paediatric ED patient toilet, opposite the main work-station. A 15-year-old female presented with abdominal pain has given birth unexpectedly. A baby is on the toilet floor attached by its cord.”
Minute One
“Baby is breathing and starting to cry, mother is alert, distraught but looking OK”. Team Leader should call for a trolley to move to clinical area. Should ask for the normal delivery pack and neonatal pack from the ER stacks and request obstetric emergency team and paediatric ED senior staff help. Cord should be ideally be clamped before moving. Do not prompt if incorrect.
Minute Two
Whole team, mother and baby should be moved to adjoining cubicles in the Resus/ER area. Prompt if this is not done (scenario cannot continue in the toilet). “The baby looks OK.”
Minute Three
Team Leader should allocate 3x team leader roles – Overseeing Team Leader (OTL) plus one per cubicle (TL1 and TL2). ED consultant could facilitate this if called. Do not prompt.
Cubicle 1, Mother – Time check, vital signs “HR 100, RR 25, BP 120/80, SpO2 96% air, GCS 15, Temp normal.” Mother to be positioned comfortably and reassured.
Cubicle 2, Baby – condition recheck. Auscultation for heart rate. “HR 120.” Resuscitation is not needed. “Baby is crying and active with a good colour.” Dry the baby and keep warm (towels and TransWarmer). Do not prompt.
Minute Four
Cubicle 1, Mother – Obstetric team has not arrived. “Mother remains alert, minimal blood loss per vaginally, cord intact, and placenta not visible if she is inspected.” TL1 to focus on 3rd stage and IV access.
Cubicle 2, Baby – Paediatric team has not arrived. “Baby’s condition is unchanged but the baby appears small.”
Minute Five
Cubicle 1, Mother – Prompt TL1 to describe what they would do next. Includes Incopads on floor, bowl for placenta, syntometrine IM. TL1 to lead discussion as to who should take over as TL1 if specialist help arrives.
Cubicle 2, Baby – Prompt TL2 to describe what they would do next. Includes assessing prematurity and getting the right equipment. TL2 to lead discussion as to who should take over as TL2.
Debrief and Feedback
You should aim to cover the following points within 5 minutes, then re-run the scenario:
Was the correct help immediately called for? (obstetric emergency team and paediatric ED senior staff)
Was there a rapid decision to move out of the toilet?
How did the team pull together?
Were TWO teams formed? (mother and baby)
Were the right stacks brought? (normal delivery stack, neonatal resuscitation stack)
Were the right actions taken to for the baby? (rapid assessment, keeping warm)
Were the right actions taken for the mother? (basic assessment, Third stage management)
Was ownership of the patients established once specialist teams arrived?
Were there any instances of:
Equipment issues?
Human factors negatively impacting communication or patient care?
Additional Resources
- Management of an Unexpected Delivery in the Emergency Department (Gupta AG, Adler MD)
- Lightning Learning: Precipitous Delivery (EM3)
- Lightning Learning: Newborn Life Support (EM3)
- Neonatal Resuscitation and the Emergency Physician (ED Central)
- Call The Midwife! (…and other tips on ED deliveries) (RCEM Learning)
- Precipitation Labour in the Emergency Department (Denise Mace)