Resus Drills: Facial Trauma
Drill pre-brief (instructor to read out)
“Welcome to this Resus Drill. Drills are for situations which are not common, and need a time-critical response. This is not a Simulation. Drills are a rehearsal for practising teamwork and speed.
We will run a scenario for 5 minutes, chat and reflect on it, then run the same scenario again for another 5 minutes.”
Assurances
Learning, NOT assessment: drills are for practice and for learning. We’re concentrating on how fast you can think, and how well you work as a team.
Safe zone: lessons are shared here, not judged, not told as tales.
5-min reflection rules: please use the debrief to be positive about what you can all do better on the re-run. These are deliberately tough scenarios. That’s the point of a drill.
Pretend it’s real: although it’s not real, we need you to help us by acting as you’d do in real life, in your normal role, and we’ll try to run it in real time.
Take-away pack: there is some information that you can take away for further learning. We recommend “spaced repetition” for the best learning!
Make some reflective notes while it’s fresh in your mind
Make yourself read them again in a couple of weeks
How does it work?
Each Resus Drill pack follows a standard format.
The drill packs are laminated and available for teaching purposes. Printable copies can be downloaded HERE.
Our drills can also be EDITED to suit your local hospital needs (Google account required).
S.E.T.U.P. (before patient arrives)
SELF… physical readiness (stay calm) & cognitive readiness (accept the challenge)
ENVIRONMENT… lighting, crowd control, appropriate equipment?
TEAM… initial briefing, identify Team Leader, allocate team roles
UPDATE… if possible, recap for the team (and yourself) before patient’s arrival
PATIENT… the patient arrives
Location of Equipment
The Facial Trauma kit can be located on the far right of the Resus/ER equipment stacks next to Bay 9 and opposite Bay 10.
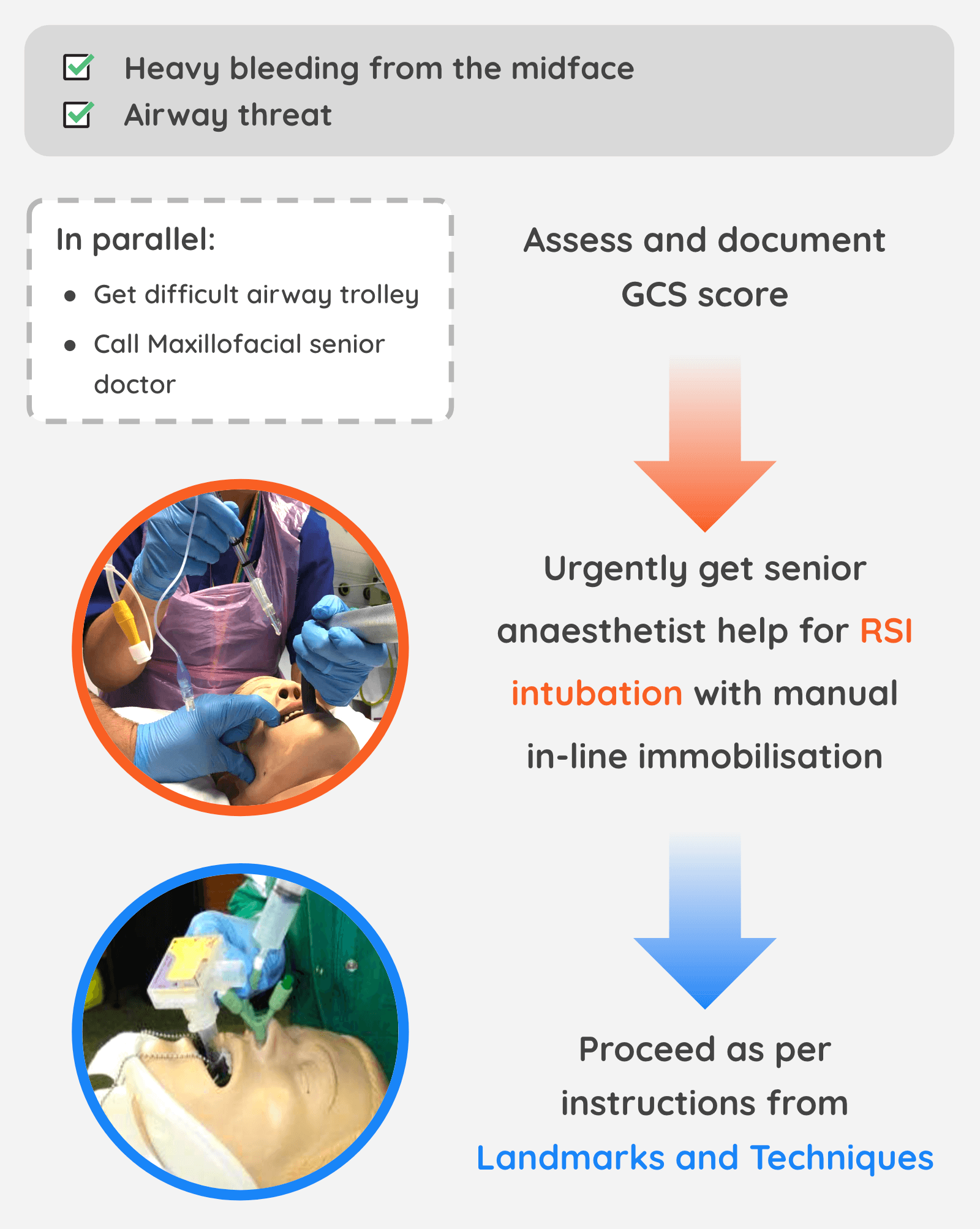
Indications
Uncontrolled midface haemorrhage due to fracture.
Intubation must be performed BEFORE this intervention
Equipment Required
Epistat nasal cannula (x2)
Bite blocks (S/M/L) (x2)
Cervical collar/Neck brace
Syringe 20 ml
Saline 100 ml
Mefix 2 cm (cut into 10 cm strips)
Landmarks and Techniques
Step 1: Insert nasal epistats into each nostril ⚠️ DO NOT INFLATE YET ⚠️
Step 2: Insert bite blocks either side of the ET tube, between upper and lower molars and with point of wedge towards the back of mouth
Step 3: Apply cervical collar to stabilise the mandible
Step 4: Inflate posterior balloons WHITE VALVE with 10 mls saline each side
Step 5: Use epistats to pull the midface forward with traction
Step 6: Inflate the anterior balloon on each side GREEN VALVE with 20-30 mls saline
Traumatic Cardiac Arrest Decision Algorithm
Red Call Sheet
Scenario Script
“The red phone has just rung with a 3-minute warning of a 49-year old bus driver, not wearing seatbelt, who has collided with a bridge. He is GCS 13 and has heavy bleeding from hitting his face on the windscreen. Here is his red call information.” (give Red Call sheet to Team Leader)
Minutes One
Team Leader designates team members and uses S.E.T.U.P. PPE and badges donned.
Should request Facial Trauma stack, Difficult Airway stack and consider activating trauma team. Do not prompt. Anaesthetist arrives if requested.
Minute Two
Paramedics arrive stating “he’s become more drowsy, blood pouring from his nose, needing a lot of suctioning” HR and BP stable.
Minute Three
Team Leader should allocate roles for intubation, primary survey, IV access and bloods. Do not prompt. If asked, “the GCS is 9.”
When airway assessed “There is crepitus of the face, heavy bleeding from nose, needing suctioning constantly.”
Team Leader should recognise need for urgent senior specialist intubation followed by midface stabilisation. Senior anaesthetist arrives to help.
Minute Four
Anaesthetist rapidly decides to intubate and achieves this quickly. MaxilloFacial team delayed in arriving (if already called).
Team Leader should decide to stabilise take action. If Team Leader waits, do not prompt, but ETT needing constant suctioning and BP starts to drop.
Minute Five
If Epistats and bite blocks inserted, bleeding is controlled. Decision made re: CT or immediate transfer. If quick secondary survey performed, no more injuries found.
Team Leader should organise senior Dr conversation to discuss imaging vs immediate transfer to Major Trauma Centre.
Debrief and Feedback
You should aim to cover the following points within 5 minutes, then re-run the scenario:
Did the Team Leader allocate roles and tasks in a way that was clearly understood? Was S.E.T.U.P utilised?
Did team members do as allocated?
On arrival of patient did Team Leader maintain team control?
Calm and clear speech?
Closed loop communication when tasking?
Body language that looks relaxed and inspires confidence?
Was the decision to control the airway with intubation and midface stabilisation taken quickly?
How did team members help the team pull together?
Were there any instances of:
Equipment issues?
Human factors negatively impacting communication or patient care?
Additional Resources
- Floating in the Face of Danger: MaxFax injuries in ED (RCEM Learning)
- Zygomatic Complex and Nasal Injury (RCEM Learning)
- Prehospital Maxillofacial Haemorrhage Control (GSAHEMS)