Resus Drills: Thoracotomy for Trauma
Drill pre-brief (instructor to read out)
“Welcome to this Resus Drill. Drills are for situations which are not common, and need a time-critical response. This is not a Simulation. Drills are a rehearsal for practising teamwork and speed.
We will run a scenario for 5 minutes, chat and reflect on it, then run the same scenario again for another 5 minutes.”
Assurances
Learning, NOT assessment: drills are for practice and for learning. We’re concentrating on how fast you can think, and how well you work as a team.
Safe zone: lessons are shared here, not judged, not told as tales.
5-min reflection rules: please use the debrief to be positive about what you can all do better on the re-run. These are deliberately tough scenarios. That’s the point of a drill.
Pretend it’s real: although it’s not real, we need you to help us by acting as you’d do in real life, in your normal role, and we’ll try to run it in real-time.
Take-away pack: there is some information that you can take away for further learning. We recommend “spaced repetition” for the best learning!
Make some reflective notes while it’s fresh in your mind
Make yourself read them again in a couple of weeks
How does it work?
Each Resus Drill pack follows a standard format.
The drill packs are laminated and available for teaching purposes. Printable copies can be downloaded HERE.
Our drills can also be EDITED to suit your local hospital needs (Google account required).
S.E.T.U.P. (before patient arrives)
SELF… physical readiness (stay calm) & cognitive readiness (accept the challenge)
ENVIRONMENT… dangers, space, lighting, crowd control, appropriate equipment?
TEAM… initial briefing, identify Team Leader, allocate team roles
UPDATE… if possible, recap for the team (and yourself) before patient’s arrival
PATIENT… the patient has now arrived
Location of Equipment
A simplified Thoracotomy kit should be located in your Resus/Emergency Room
A full surgical thoracotomy kit should also not be too far away from the simplified kit
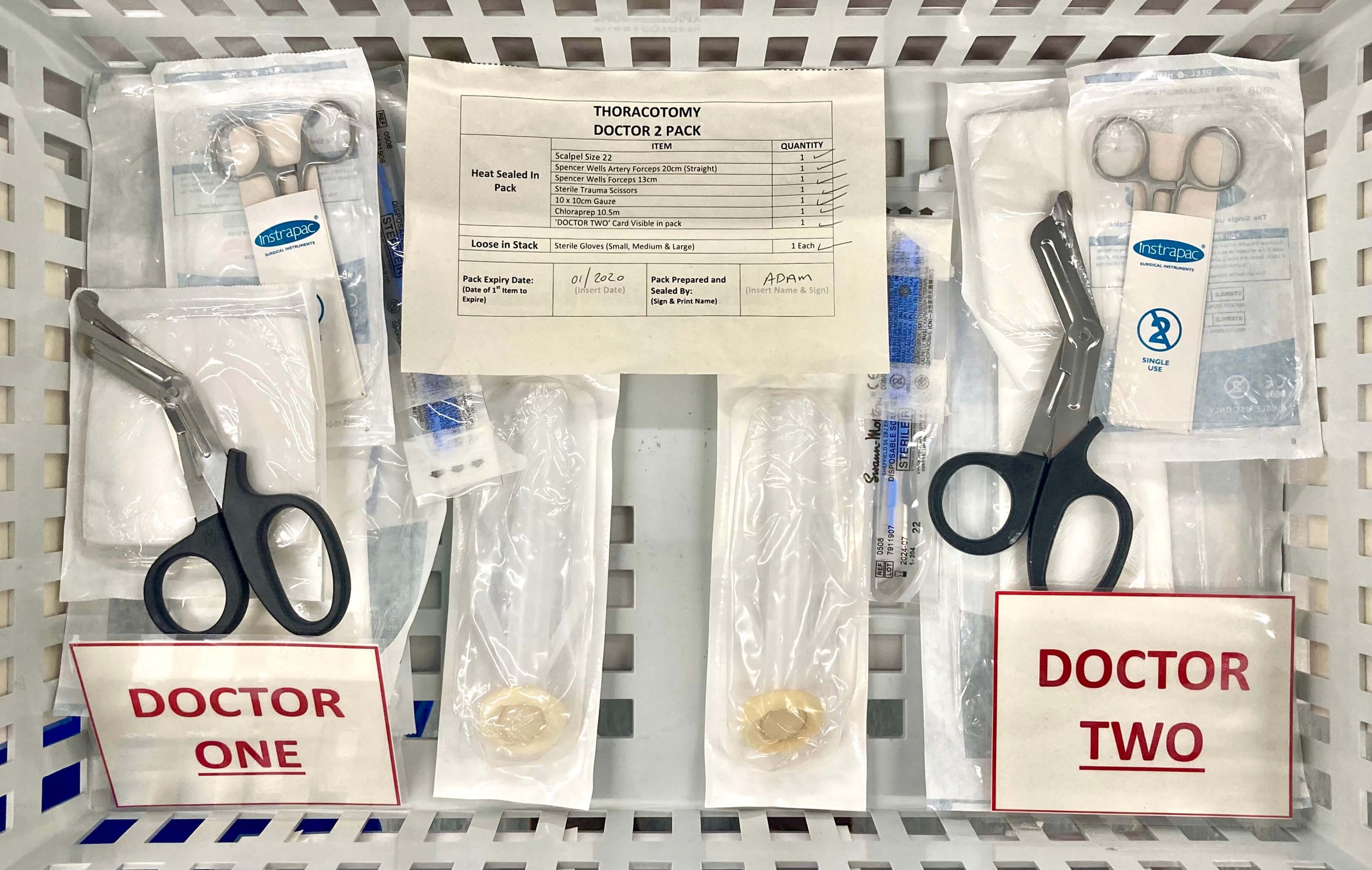
Here’s what the inside of a simplified thoracotomy kit looks like
Indications
Cardiac arrest after a penetrating thoracic injury AND downtime of <15 minutes
Equipment Required
Sterile scalpel blade (size 22)
Spencer-Wells artery forceps (20 cm straight)
Spencer-Wells forceps (13 cm)
Sterile trauma scissors
10x10 cm Gauze (to protect against sharp ribs)
Chloraprep applicator 10.5 cm
Drugs for anaesthesia
Full thoracotomy kit on standby (including rib spreader, Gigli saw)
Landmarks and Techniques
Step 1: Concurrent intubation and IV access
Step 2: Thoracostomy incisions are made on both sides but extending to the posterior axillary line – confirm thoracostomies haven’t achieved ROSC
Step 3: A skin incision (down to muscles) is made across the anterior chest wall joining the 2 thoracostomy incisions, passing over the sternum
Step 4: Intercostal muscles are divided using tough-cut shears +/- scalpel
Step 5: The sternum should be divided using the tough-cut shears
Step 6: The chest wall, if incised correctly, will open upwards exposing the internal organs
Step 7: The pericardium is identified and an incision made vertically in the centre of the pericardium
Step 8: Any clot of blood needs to be evacuated manually from the pericardial space
Step 9: If there is no spontaneous cardiac activity, internal compressions should be commenced
Step 10: Bleeding from wounds to the heart are usually stopped using thumb/finger pressure
Step 11: Bleeding points from the chest wall may need to be tied by the second team member using the vicryl suture
Step 12: Pre-alert the cardiothoracic team for immediate transfer
Traumatic Cardiac Arrest Decision Algorithm
Red Call Sheet
Scenario Script
“The red phone has just rung with a 3-minute warning of a 19-year-old male stabbed in the epigastrium. Here is the red call information.” (give Red Call sheet to Team Leader)
Minutes One & Two
Team Leader designates team members and uses S.E.T.U.P. (Self, Environment, Team, Update, Patient arrives). Gloves, aprons, role badges, ED thoracotomy kit, O neg blood and rapid infuser fetched. Trauma alert activated (no-one arrives until scenario over).
Minute Three
Paramedics arrive stating that he’s just lost his cardiac output. Decision to do clamshell needed. CPR/adrenaline should not be initiated – should be verbalised to team as deliberate decision. Arrest time should be noted. Team members allocated for: thoracostomies (x2 senior doctors + assistant), intubation (x1 + assistant), IV / IO access (x2), activating massive haemorrhage protocol.
Minute Four
Nursing staff should set up rapid infuser. Member of staff should be allocated to phone in cubicle, to liaise with transfusion and others. Thoracostomies performed – no rush of air, lungs are inflated. If intubation is attempted, it is easily achieved.
Minute Five
Team Leader should decide rapidly to perform full thoracotomy and allocate one senior doctor to each side of the chest.
Instructor announces that we have fast-forwarded three minutes and that the heart is empty, feeble beats, no pericardial tamponade or RV wound found.
Team Leader should review time since cardiac output was lost and verbalise and agree with team the decision to stop transfusion / resuscitation if no skilled help has arrived within 15 mins of onset of cardiac arrest.
Debrief and Feedback
You should aim to cover the following points within 5 minutes, then re-run the scenario:
Did the Team Leader allocate roles and tasks in a way that was clearly understood? Was S.E.T.U.P utilised?
Did team members do as allocated?
On arrival of patient did Team Leader maintain team control?
Calm and clear speech?
Closed loop communication when tasking?
Decision to attempt thoracotomy taken quickly?
Key roles achieved?
Correct (ED) thoracotomy kit fetched?
Patient intubated?
Two people allocated to perform thoracostomies then clamshell?
Staff identified for transfusion (rapid fluid infuser, O-negative, massive haemorrhage protocol activation, team member to communicate with lab)?
Did the Team Leader sum up and decide appropriately to stop resuscitation?
Were there any instances of:
Equipment issues?
Human factors negatively impacting communication or patient care?
Additional Resources
- Emergency thoracotomy: "how to do it" (D. Wise et al.)
- Procedural Aide Memoires – PAMs: Resuscitative Thoracotomy (MAGPAS)
- Crack the chest. Get crucified. (J. Hinds)
- Epidemiology and aetiology of traumatic cardiac arrest in England and Wales (E. Barnard et al.)
- DIY Thoracotomy Trainer (SimGHOSTS)
- Low Cost, Low Fidelity Simulation Model for Teaching Thoracotomy (A. O’Connell et al.)
- Pre-hospital management of life-threatening chest injuries (RCSED)
- Pre-hospital physician-performed resuscitation procedure that can yield good results (G. Davies et al.)
- Thoracotomy (PHEMcast)