#SimBlog: SVT
““17-year-old has felt palpitations for a couple of hours. Breathing feels slightly tight but has not collapsed.””
Observations
A – Patent, Talking
B – Bilat Air Entry, Sats 100% on Air
C – HR 210, BP 110/65
D – Alert
E – Temp 37°C
Clinical Findings
Slightly clammy
Why We Simulated?
SVT is often described as "like the buses": you go around without seeing any, and then three turn up at once. It is seen in both adults and children. Understanding the management and the signs of compromise is important so that the treatment is escalated appropriately.
In the stable patient it may resolve with some simple and non-invasive techniques (check out the results of the REVERT trial summarised in 'Further Resources').
It is also necessary to think about the management beyond ED as it can be easy to cardiovert the patient (either chemically or electrically) and then discharge them without thinking what happens next.
Further Reading:
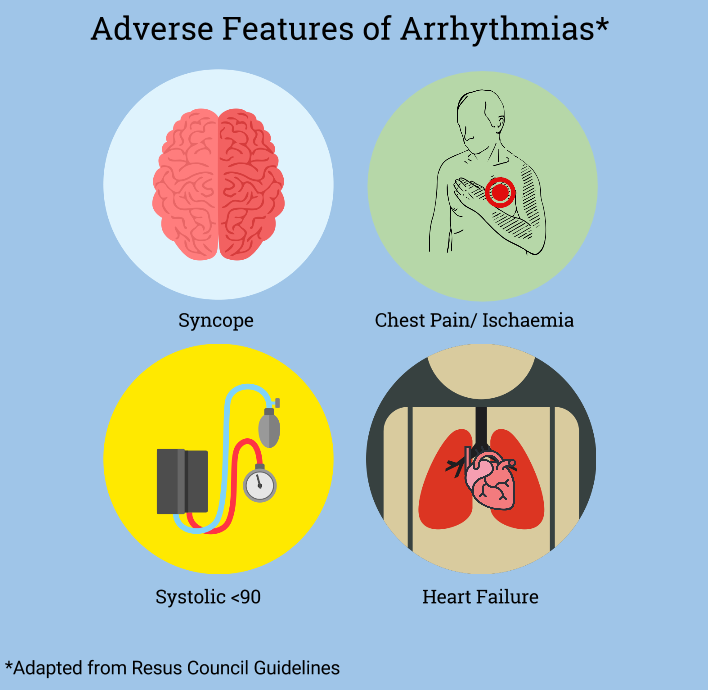
- Resus Council UK – Peri-Arrest Arrythmias
- RECM Learning – Tachycardias in the Resus Room
Learning Outcomes
Be familiar with emergency equipment such as the defib – and how to change between leads/paddles.
Consider defib safety/hazards such as water on floor and oxygen.
Know your emergency doses – electricity included. How many joules do you use for a DC cardioversion?
Positive Feedback
Escalated management from valsalva to adenosine.
Recognised deterioration and indication for DC cardioversion.
Repeated reassessment with ABCD approach.