#SimBlog: Ventricular Tachycardia
““A 65-year-old male has self-presented to the ED with a history of palpitations for 2 hours. No chest pain or SOB.””
Observations
A – Clear & self maintaining.
B – Rate 15, SpO2 98%.
C – Pulse 200, BP 110/75.
D – E4 V5 M6 pupils equal
E – Temp 35.9°C
Clinical Findings
Broad Complex Tachycardia
Initially no adverse clinical features
Why We Simulated?
Arrhythmia is a common presentation to the ED, recognition of a stable/unstable arrhythmia is crucial in deciding the next steps in the patient's management.
In the event of cardiac arrest standardised management will give the best chance for Return of Spontaneous Circulation (ROSC)
Further Reading:
Learning Points
Four signs of unstable arrhythmia – Chest Pain, Hypotension (BP<90), Signs of Heart Failure, Syncope/ LOC.
Spotting a deterioration in the clinical condition can come from any member of the team but should be communicated effectively.
If issuing an instruction and you don’t know the persons name physical contact can make sure they acknowledge you.
Cardiac arrest in a shockable rhythm should be defibrillated as soon as possible.
Avoid task focus or being “hands on” if leading.
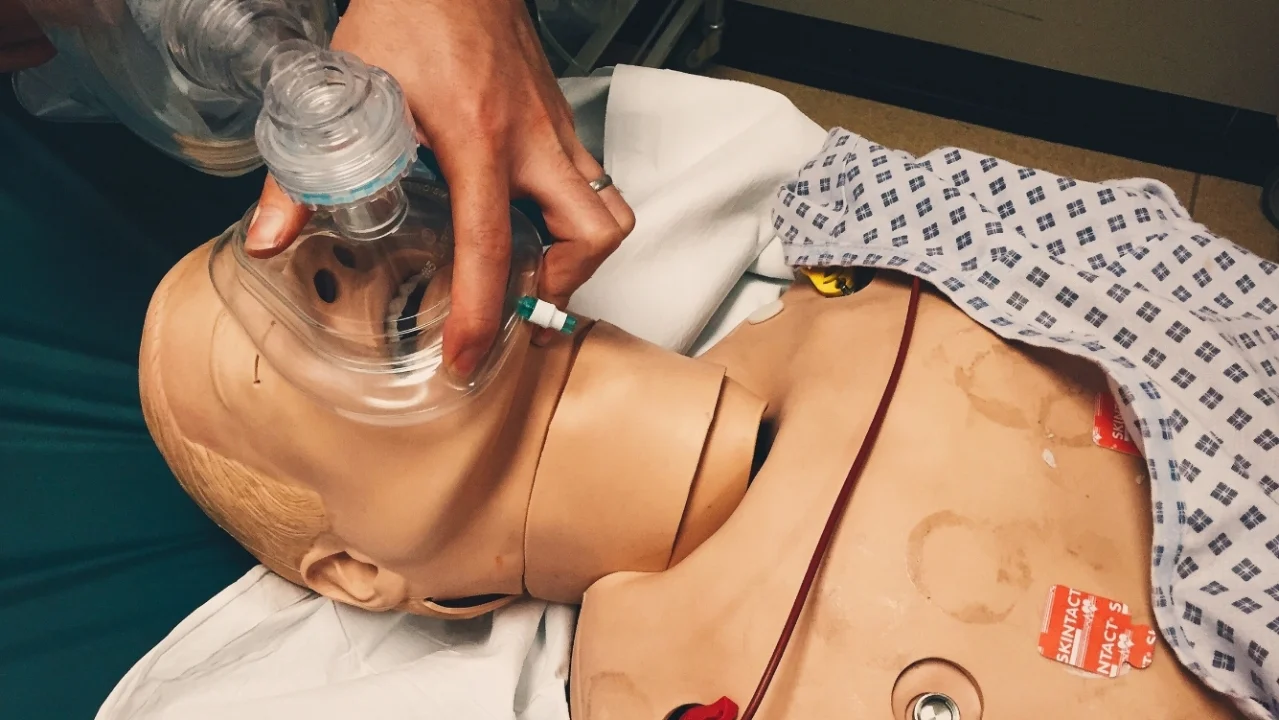
Compressions should be 30:2 unless there is a definitive airway (ETT).
Positive Feedback
Early recognition of initial arrhythmia and potential for decompensation.
Identified need for senior intervention.
Medication requested and delivered in a timely manner.
Identified quickly went into cardiac arrest and acted accordingly.