#PEST2015: Meningococcal Sepsis
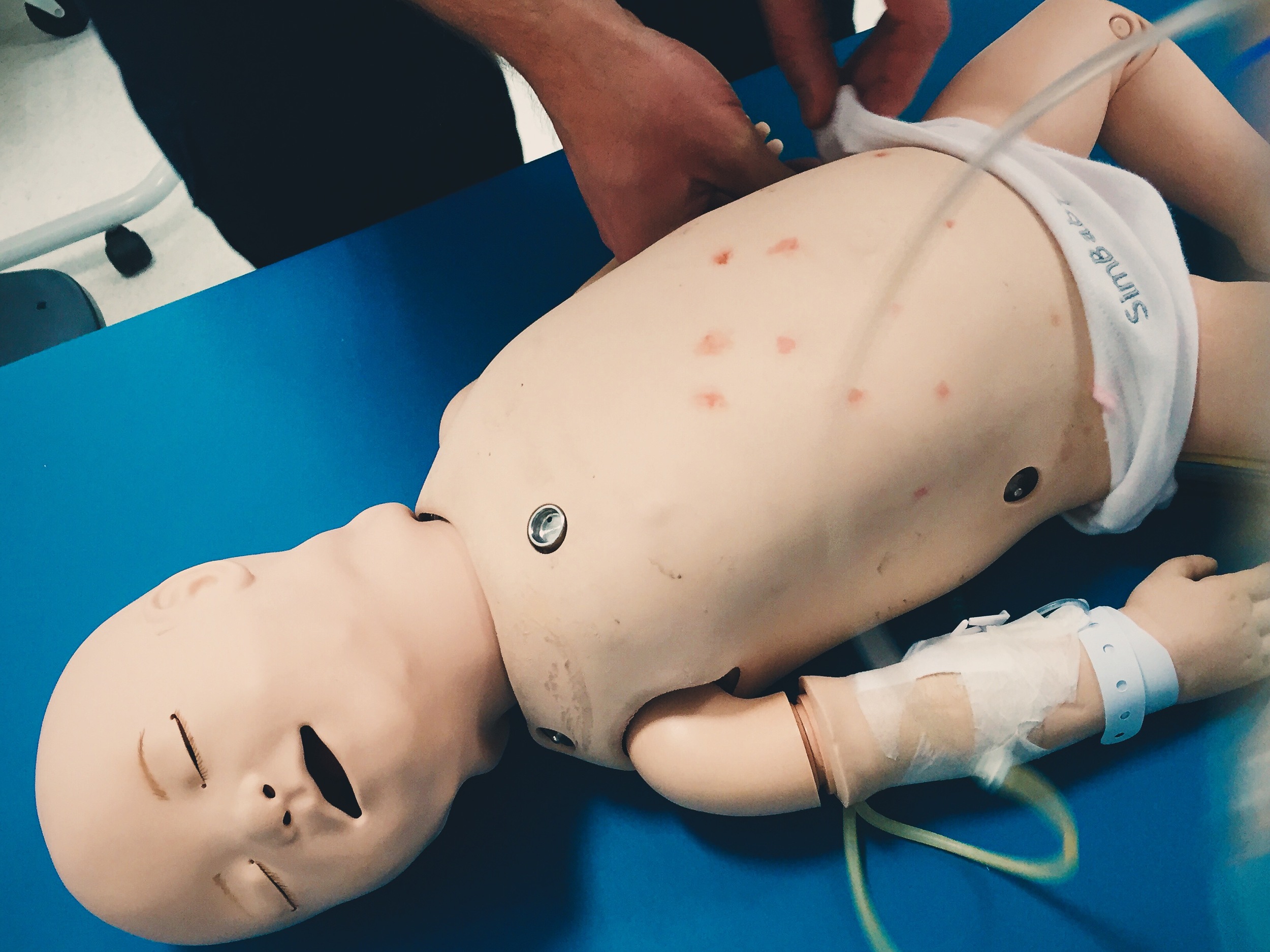
““9-month-old unwell & febrile at 39deg, HR 190, peripherally shut down & lethargic.””
Observations
RR – 60
SpO2 – 88% in air
HR – 190
BP – 70/40
CRT – 5 secs
Clinical findings
Responds to pain.
Cold hands & feet – very shut down peripherally.
Non blanching rash to torso.
Why we simulated?
In the child with septic shock timely identification, fluid resuscitation and antibiotic administration are key – delays in antibiotic administration can significantly increase mortality.
Learning outcomes
Try to “look forward” when managing patients; have fluid boluses/drugs drawn up ready in advance .
Share your mental model – verbalise what you are planning/thinking then the whole team is in the loop and working towards the same goals.
In sick shut down patients IV access is likely to be very difficult initially, consider IO as first line.
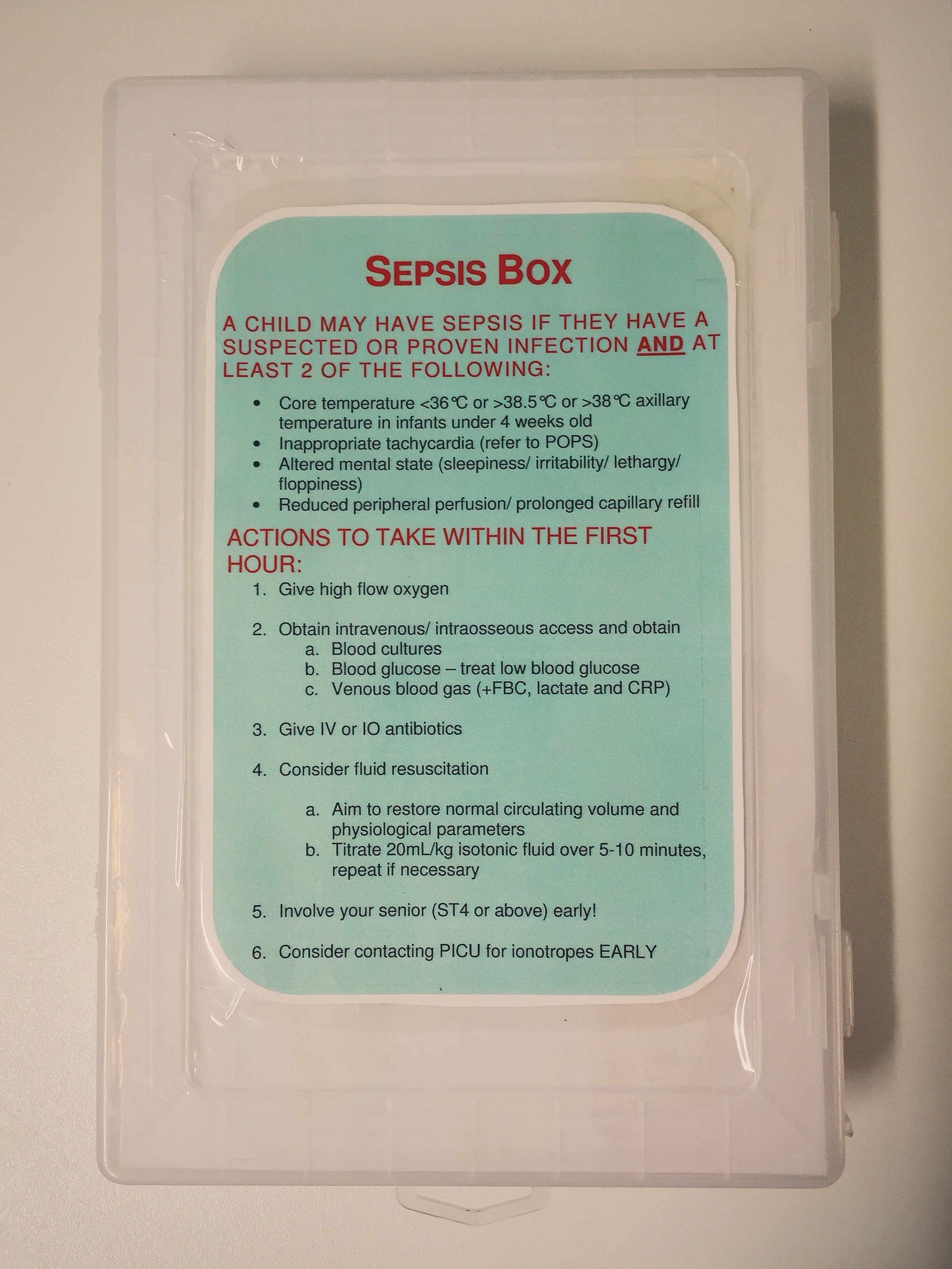
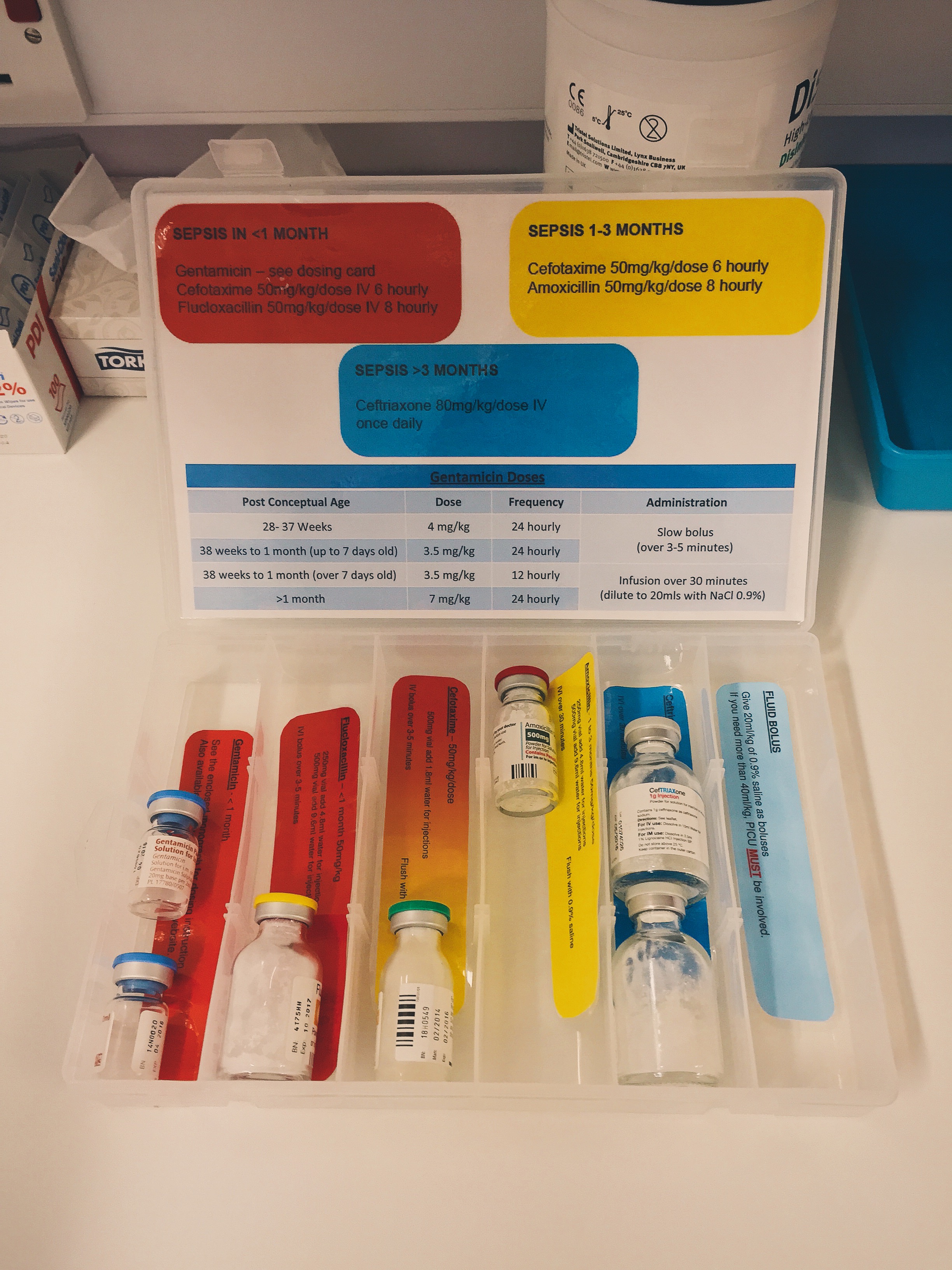
Use our “Sepsis box” – it’s a one stop shop for the antibiotics we use most commonly including drug protocols and guidelines.
Positive feedback
Early identification of serious bacterial infection.
Prioritisation of antibiotics and fluid resuscitation.
Fluids and antibiotics administered within 10 minutes of patient arrival.