Delirium
“Many patients, when they come to a hospital, they enter through the emergency department. That is their portal of entry. That is their first stop. The emergency room is a very busy place with a high turnover. It’s not an ideal place for recognizing, let alone treating, delirium.”
The Audio
What is Delirium?
There are many terms used to describe patients with delirium: “confused”, “acute confusional state”, “knocked off” are just a few and I am sure you will have heard others used.
Why is Delirium a problem?
If a patient develops delirium, it means they:
are more likely to die
stay in hospital longer
have an increased likelihood of developing dementia
have worse outcomes (Increasing risk of Nursing Home care upon discharge)
Have increased levels of distress (~80% experience distressing recollections)
Types of Delirium
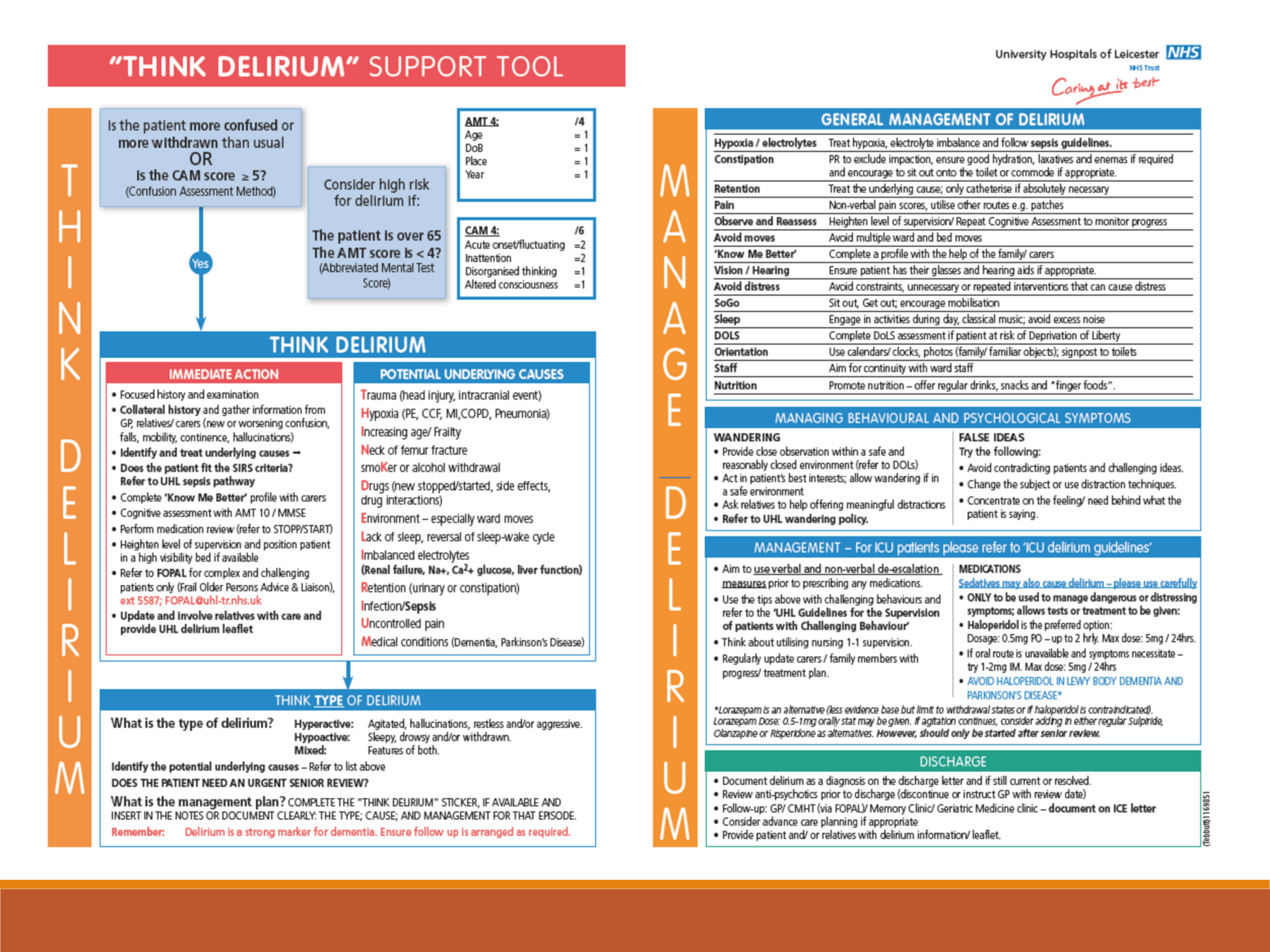
Hyperactive (agitated, hallucinations, restless and/or aggressive)
Hypoactive (withdrawn or drowsy. This type is more common but difficult to detect and is associated with higher risk of mortality.)
Mixed (mix of above)
Causes of Delirium
Often multifactorial – constipation, pain, dehydration, hunger, infection and/or illness, medications, urinary retention, environment, lack of cues for orientation (e.g. clock/calendar) can all contribute.
The cause of delirium may not be obvious in the ED – accepting uncertainty in acute setting is important.
Identifying Delirium
Identification of delirium is a key; therefore screening in the ED is important for initial recognition and early interventions. Different types of screening tools are available and currently most suitable tool for ED environment is being assessed. Failure to detect delirium in the ED is associated with increased mortality and is an independent predictor of increased hospital stay (currently 70% of delirium is not picked up in ED).
Rapid screening in the ED: ask “Months of the year, backwards” and “What is the day of the week?”
When used in combination a study showed it identified 93% of delirium cases.
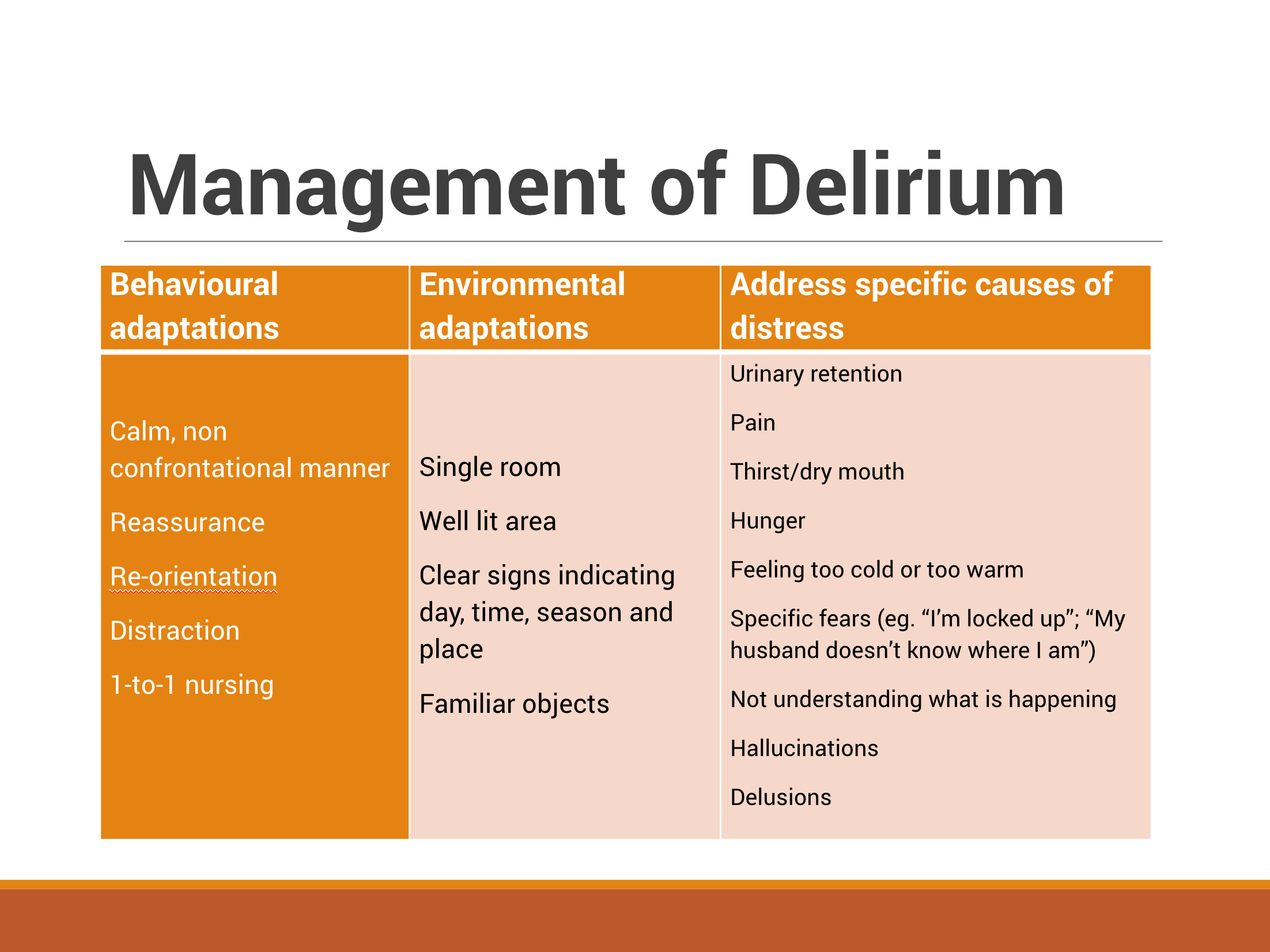
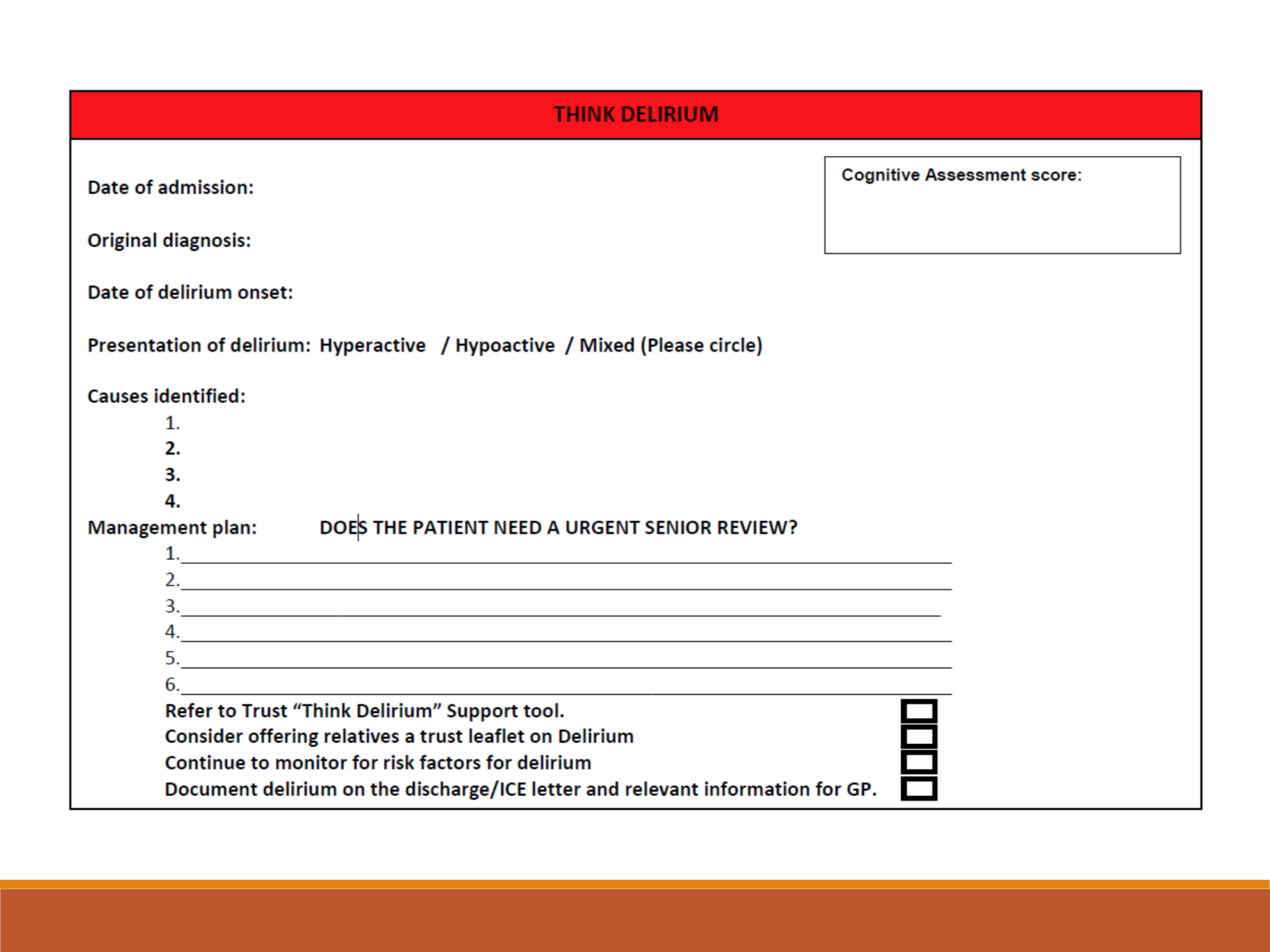
Management of Delirium
There are several interventions that can be made and we should try address these in the ED.
Behavioural adaptations (calm manner, reassurance, re-orientation etc.)
Environmental adaptations (single room, well lit area, clear signs indicating time & day etc.)
Treat underlying causes (pain, thirst, urinary retention, constipation, infection etc.)
ED Pitfalls:
ED is a very “deliriumogenic” environment: it is busy and noisy with long waits in chairs or on trolley. There are numerous investigations and movement. Patients may be exposed to a lack of sleep, non-natural lights, and disorientation as to the time of the day. Patients will encounter multiple people in a short period of time.
The Slides