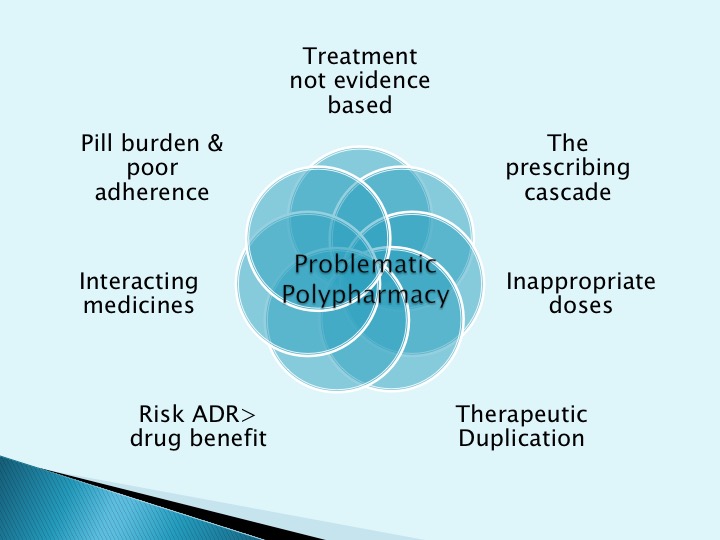
Polypharmacy
“The human’s “desire to take medicine” carries, however, a price tag. Nature’s maladies are succeeded by iatrogenic hazards. Arising out of a restorative instinct, polypharmacy becomes itself an affliction.”
Seven steps to managing polypharmacy in practice
This week we are attempting a slightly different format for the summary of the IPE session. The audio from the meeting has been recorded and embedded below, along with the slide set used.
We have also included some links below for some of the resources discussed.
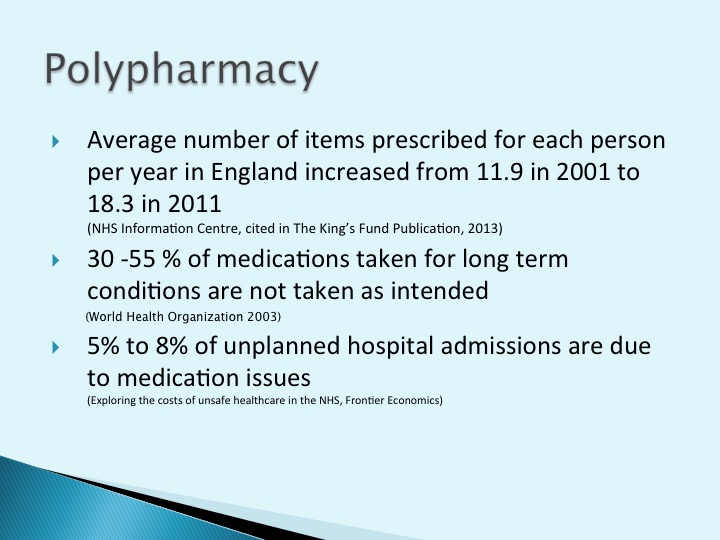
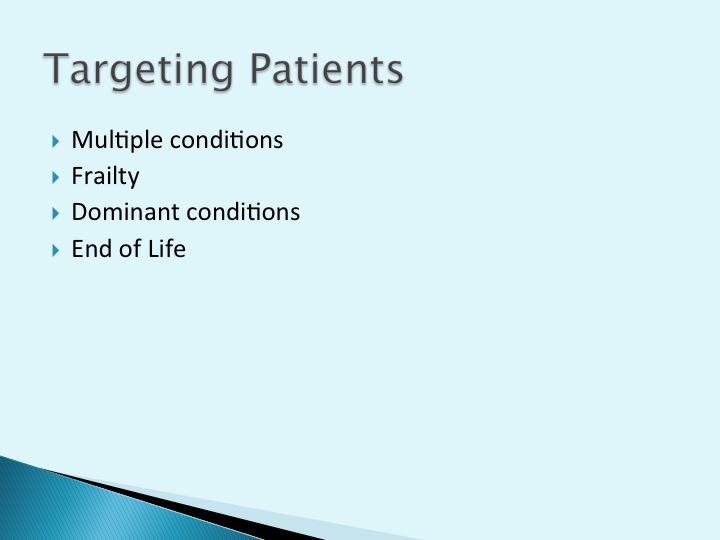
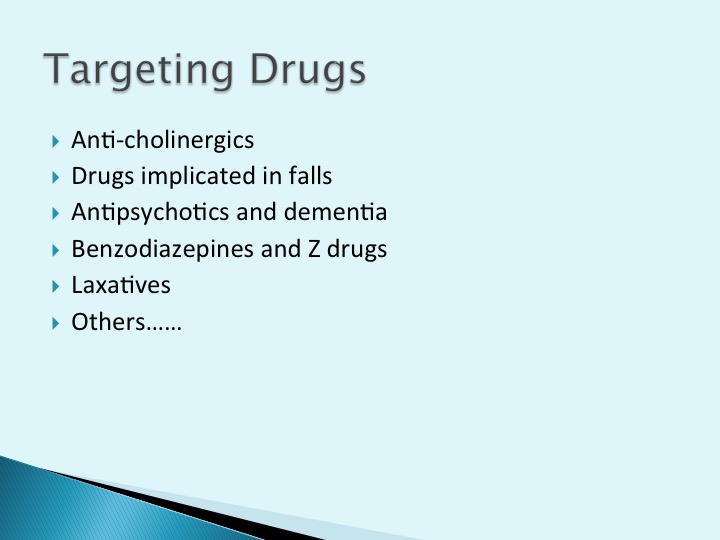
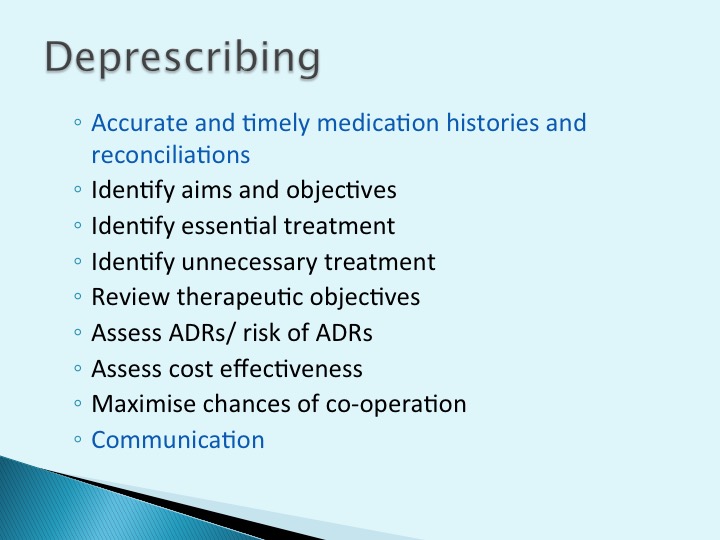
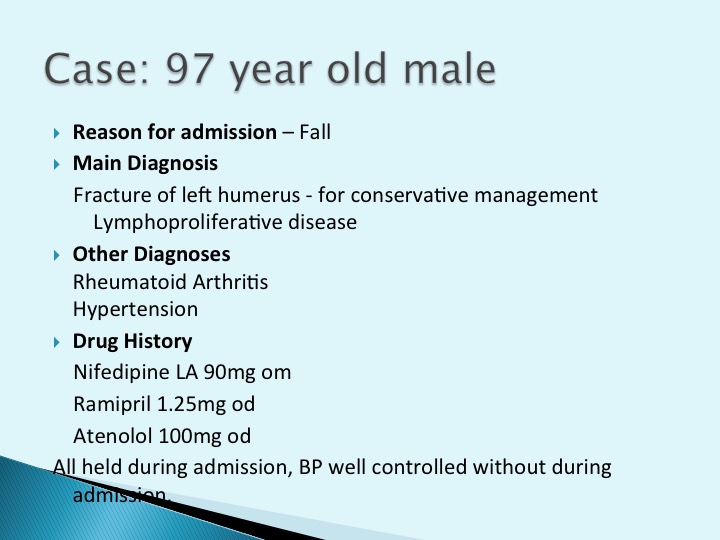
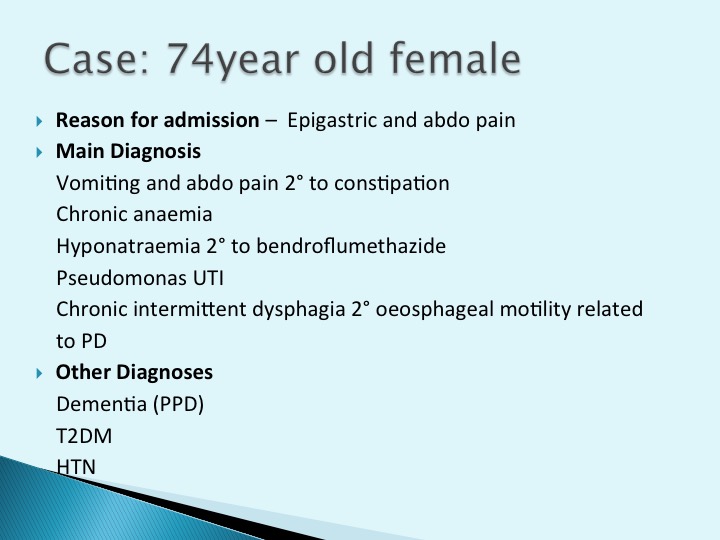
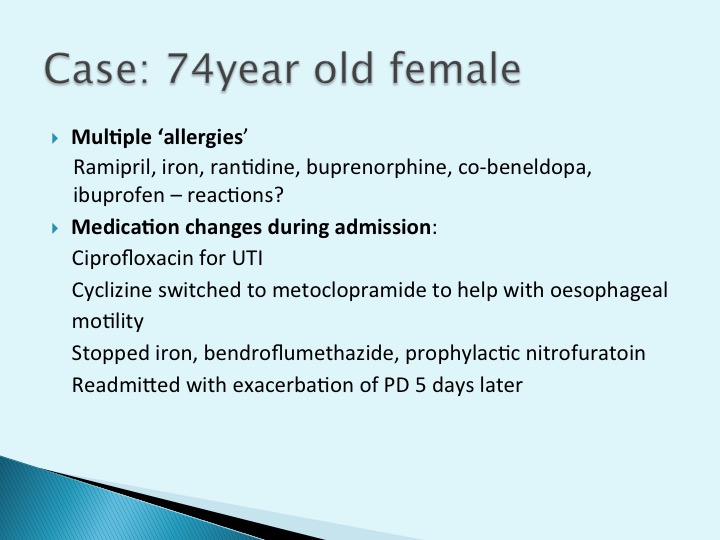
This session looks at some of the challenges of patients on multiple medications and some of the things we can do to manage this problem. The role of various professionals including doctors and pharmacists is discussed, but as always there are several problems identified that need to be overcome.
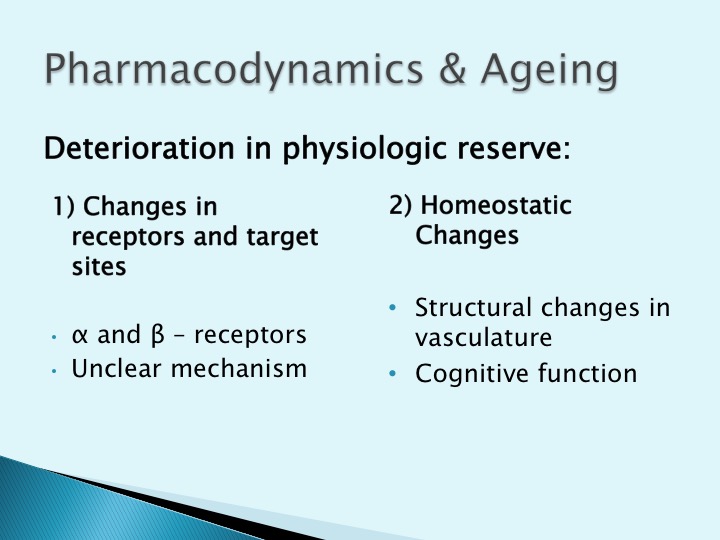
Why is this relevant to the ED? HAP 35 Complex Older Patients includes: "Describes the requirements for altered prescribing in the elderly and recognises the effects of polypharmacy".
ED Pitfalls:
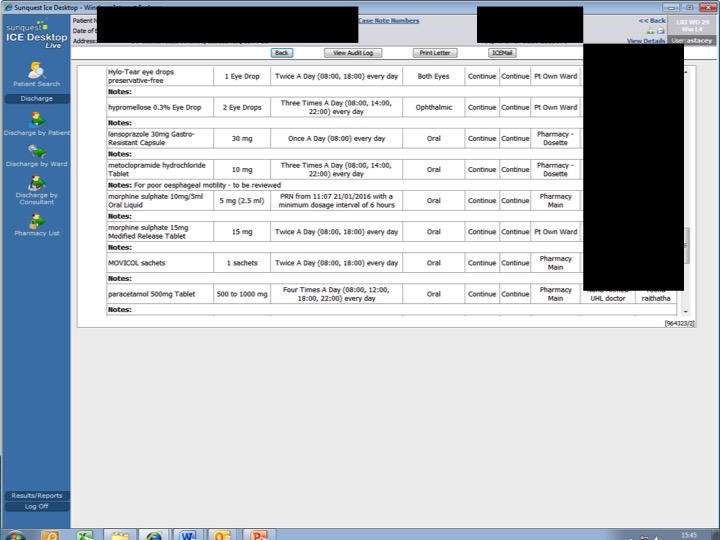
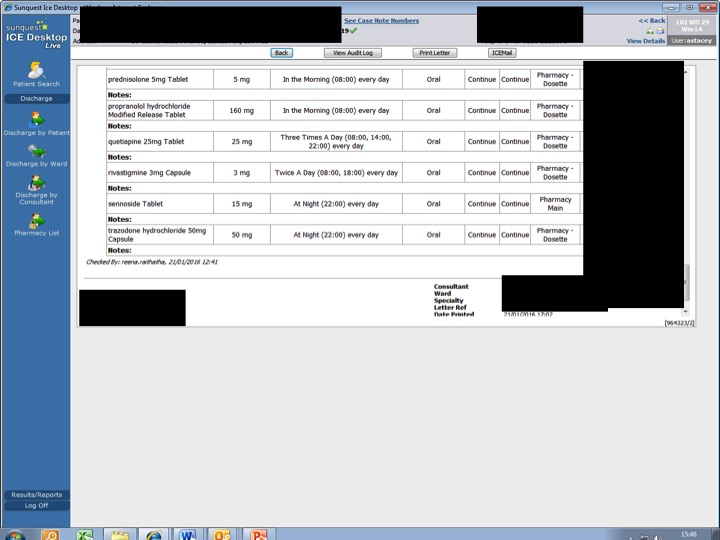
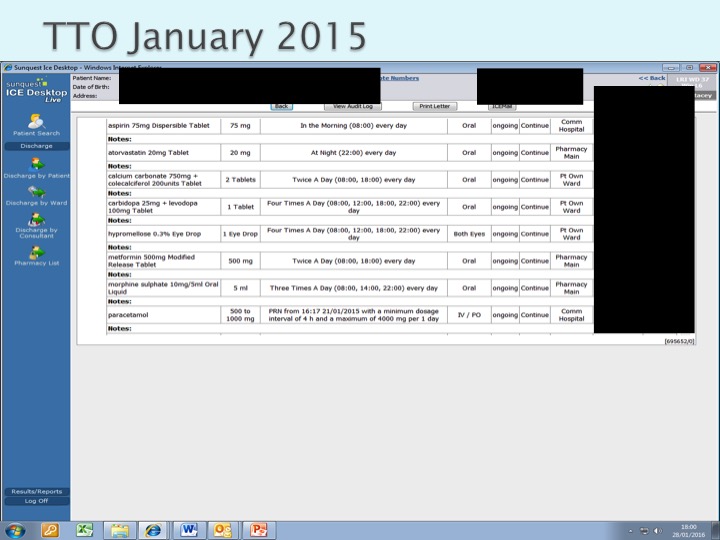
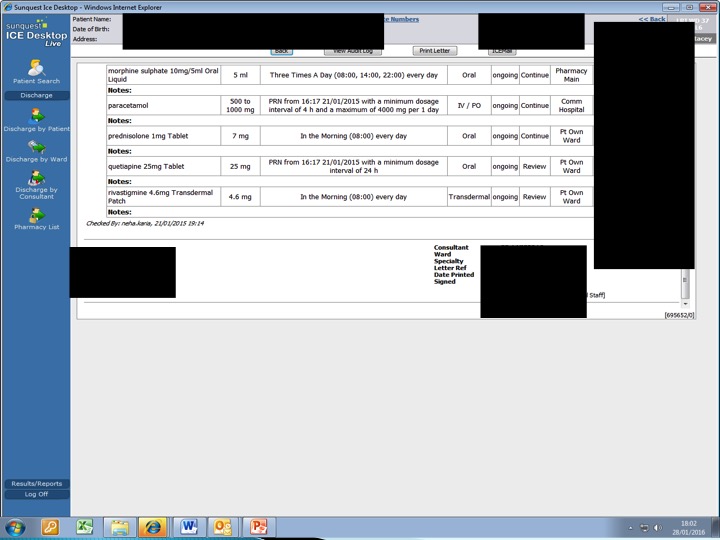
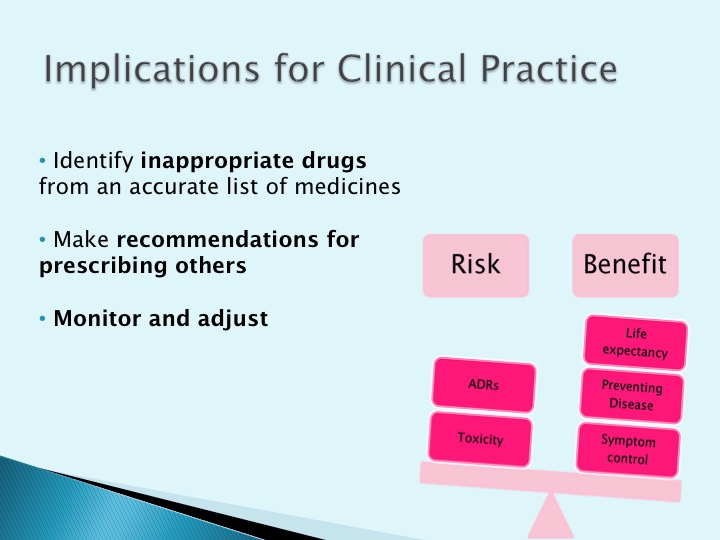
- Full Drug History: This can be difficult to establish in the ED as there can be limited information and other time critical intereventions are needed. Is there a role for Pharmacists in ED?
- Can I really deal with this in the ED? This is open to debate, but realistically we do have an obligation to consider if drugs are causing problems. If you are altering meds or discharging a patient it is important to write to their GP, part of this can be to suggest a medication review.
The Audio
The Slides
Resources:
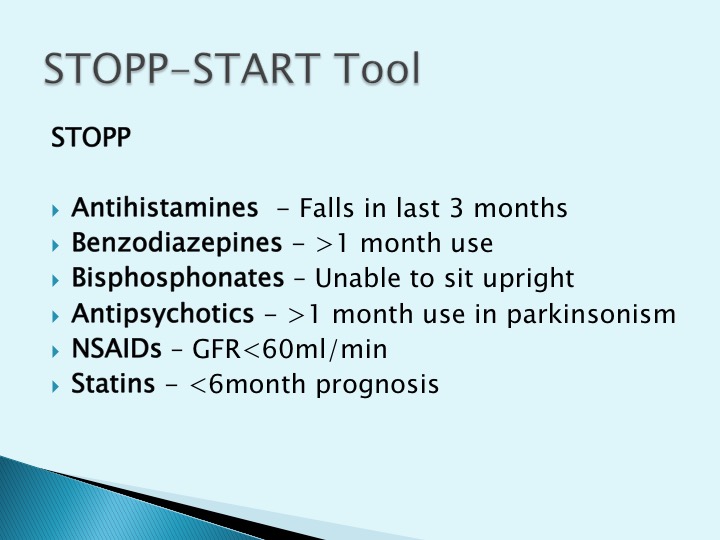
- STOPP/START Toolkit – NHS Cumbria
- Beers Criteria for Potentially Inappropriate Medication Use in Older Adults (2012) – The American Geriatrics Socitey