Mobility Assessment
“Birds have wings; they’re free; they can fly where they want when they want. They have the kind of mobility many people envy.”
How can we do baseline mobility assessment?
Anyone (Nurses, PCCs, doctors etc.) can initiate basic mobility assessment with following recommendations:
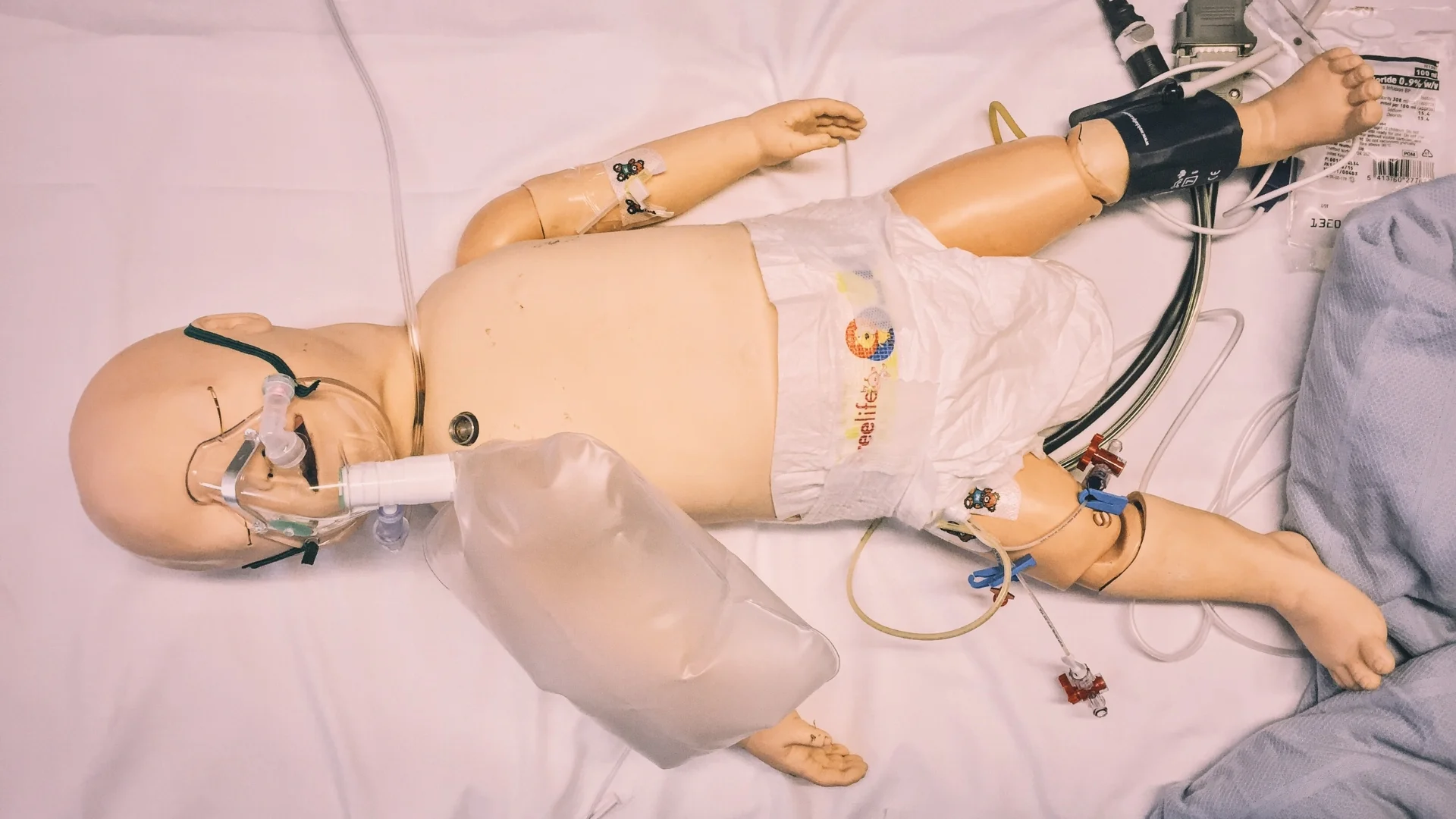
GET UP & MOVE: A way to check if a patient is safe to attempt standing and walking is to ask them to do a straight leg raise whilst lying supine. If they are able to do this then they should have adequate lower limb strength to attempt standing and walking.
1min STAND: Timed unsupported stand (stand unaided for 1 minute) can be useful; patients who can stand for less than 1 minute are at high risk of falls this is particularly useful for ED physicians working with limited time and space.
3m WALK: If medical staff can do one special test when assessing frail older patients, Timed Up and Go (TUG) test is the most useful: ask a patient to rise from the chair, walk 3 meters, turn around and return to the chair. Patients who take longer than 15 seconds require a physiotherapy assessment. If you are doing these assessments, communicating the results to the PT is a key! Watch a demonstration in the embedded video.
DUAL TASK: getting a patient to walk and talk at the same time can be a useful indicator of patients at increased risk of falls: if they cannot dual task their falls risk is high.
- Before referring to physio make sure your patients receive adequate analgesia and Parkinson’s medications if indicated prior to physio assessment to ensure accuracy and efficiency of assessment.
- For patients with Parkinson’s disease cueing (verbal, visual and audio) helps stimulate movement through accessory pathways in the brain. This is a non-pharmacological and evidence based way of improving mobility.
- Trolley Height: trolleys in the ED are often too high to get on an off easily. This makes it difficult to assess patients in the majors area. The new ED will have more appropriate trolleys and this is already written into the frail friendly design of the department.
What We Offer
Good communication and accurate baseline assessments from other clinical staff can help the physiotherapy team work more efficiently and ensure referrals have realistic goals.
“EFU (Emergency Frailty Unit) has a dynamic MDT working environment and can be a model for others.”
The following can be accessed in our department:
Physiotherapy Assessment: Prior to assessment, they create a problem list from case note review and verbal communication from medical and nursing staff. They use the UHL standardised assessment tool (SOAP format – Subjective, Objective, Assessment/Analysis, Plan).
Rapid Assessment and Discharge (RAD) Team: Physiotherapist and OT service in ED, EDU, AMU and AFU to expedite safe discharge. Available Mon-Fri 8:00-16:30. See attached poster for referral criteria. Bleep 4304 (physio)