#SimBlog: Feeling The Heat?
““Terry (71) was out in the garden watering his potatoes when he felt unwell and collapsed. He had a 30sec LOC.””
Observations
A – Patent
B – Good Bilat Air Ent, Sats 97%
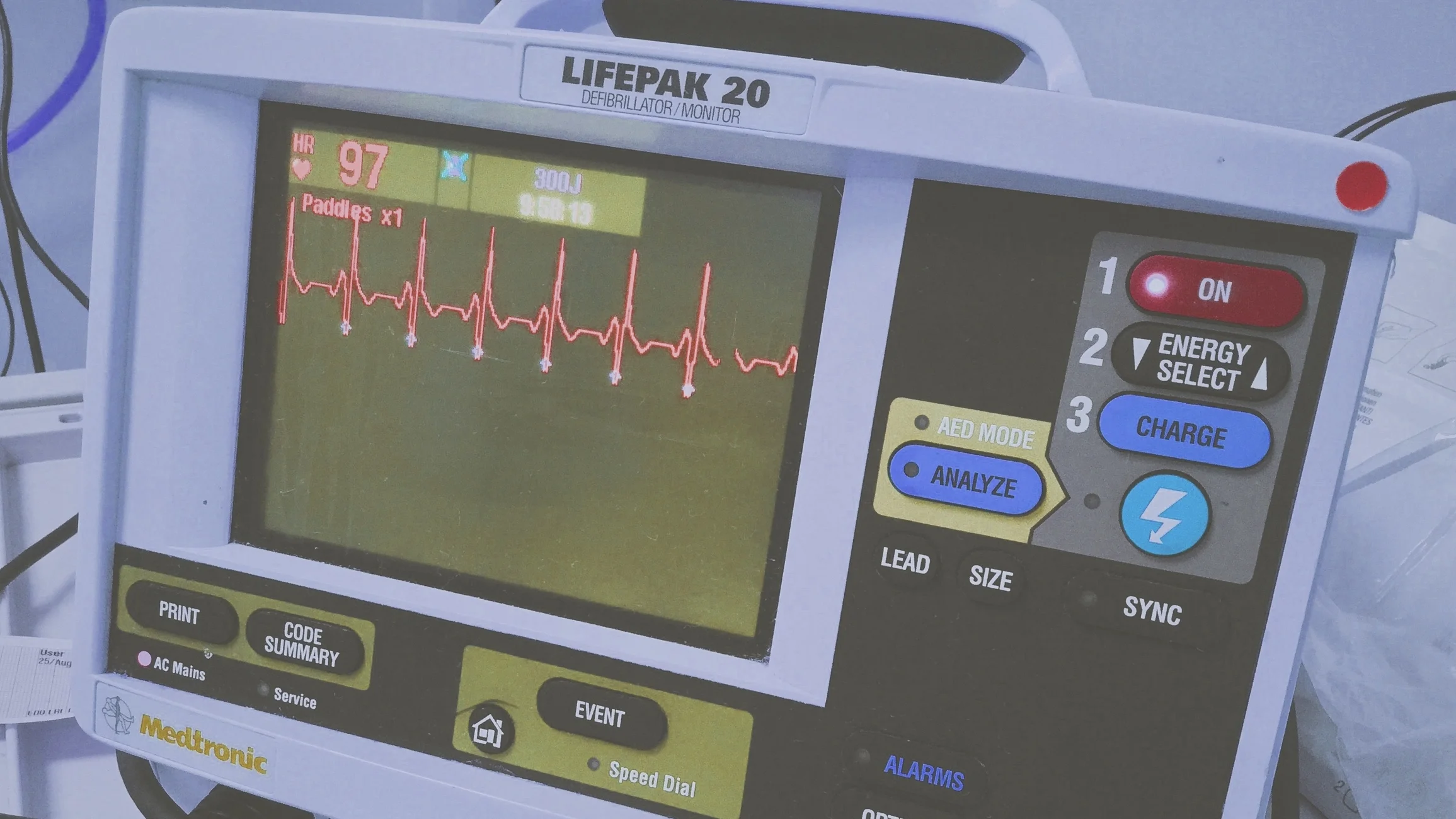
C – HR 96 (AF) BP 106/75
D – GCS 15
E – Temp 37.4°C
Clinical Findings
No injuries
Slightly sweaty
Why We Simulated?
In the UK we love to complain about the weather, however when we do get sunshine and heat it can take us by surprise!
The current heatwave (this sim was run on 20/7/16) has already led to several presentations in our department with heat illness.
It may simply be, as in this case, that over exertion and dehydration can cause a collapse (most likely through vasodilatation). Alternatively it can be far more serious...
Our bodies primarily lose heat through evaporation, if the ambient temperature (and humidity) become too high this mechanism fails & body temperature rises, leading to HYPERthermia. This goes on to affect multiple body systems including: CNS disturbance, renal failure, rhabdomyolysis, vasodilation (and even shock).
This process is known as Heat Stroke and can be divided into two different aetiologies:
1) Classical (non-exertional)
Often older patients (>70yrs)
Underlying medical conditions (or medications) impair the persons ability to thermoregulate or to remove themselves from the hot environment or access hydration.
Anticholinergic medications
Diuretics
Poor mobility
Cognitive impairment
Recreational drugs
2) Exertional
A leading cause of death for young athletes.
Often otherwise healthy individuals.
Risks include:
Strenuous exercise in high temperature & humidity
Lack of acclimatisation
Poor physical fitness
Obesity
Dehydration
Look for CNS dysfunction, a temperature >40°C, and evidence of other organ dysfunction. A history of exposure to heat is also important (without this you need to think carefully about other reasons for this presentation).
Mortality for Heat Stroke can be high (Life in the Fast Lane quote >60%).
Management is rehydration and supportive therapy, Critical Care may be needed to support organ dysfunction.
Learning Points
Have faith in your assessment, if your patient appears well they probably are.
Consider using tools such as SBAR when handing over or seeking advice.
The bair hugger has an ambient temperature that can be used for cooling.
Positive Feedback
Good pre-allocation of roles.
Opened discussion to whole team with regards to management or concerns: "Is there anything else anyone can think of?"
Considered the possibility of sinister causes of collapse in this age group.
Further Reading:
- UpToDate®: Classical Heat Stroke (requires subscription)
- UpToDate®: Exertional Heat Stroke (requires subscription)
- LITFL: Heat Stroke