#SimBlog: The One Where They Turn Out To Be A Child…
““Approx. 18-year-old male, witnessed to collapse and have a seizure in town. When he wakes up he tells you he’s only 15.””
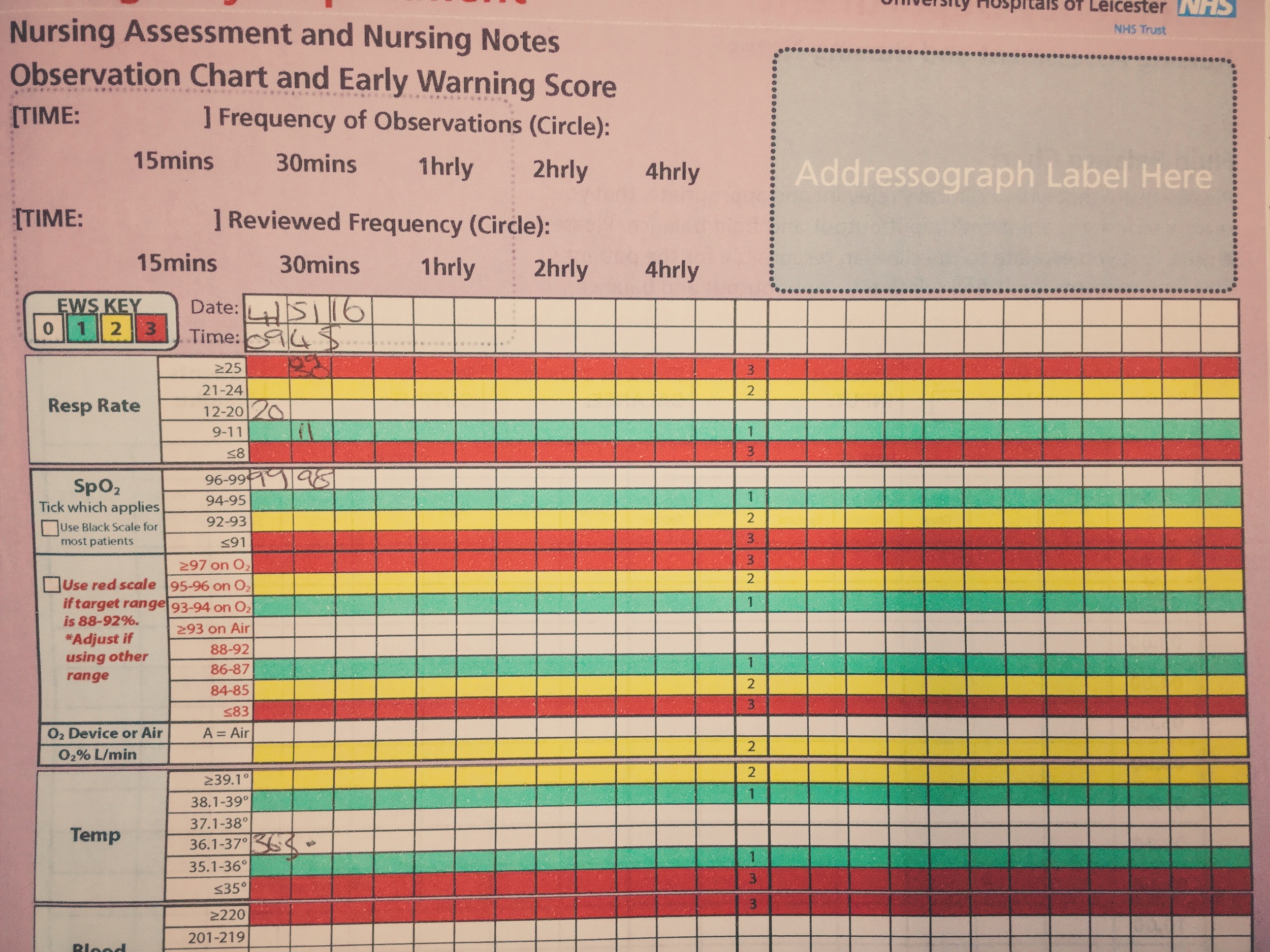
Observations
A – Patent
B – Chest Clear, Sats 99%
C – HR 104; BP 110/56
D – GCS E3 V3 M4 BM 6.5
Clinical Findings
No signs of injury
Has been incontinent of urine
Has a bank card with a name on
Why We Simulated?
Information pre-hospital can be very limited, a patient with reduced GCS may have no way of confirming their identity. In this case we used the "age" as a surprise, however advanced care plans or past medical history can also catch you out. It is sometimes necessary to try and find other sources of information.
St. Emlyn's have previously discussed the ethics of unlocking a patient's mobile phone. For those working in the ED it is worth knowing that certain models (iPhones) can hold vital information.
As a final point, from a pragmatic point of view, if adult staff are faced with an unwell child but are unsure of what to do the following is a reasonable approach:
Call for help (in our centre a paediatrician is never too far away!)
Fall back to an ABC approach.
If immediate threats to life are present consider managing the patient as you would an adult – for example using the adult ratio of compression to ventilation in BLS/ALS is better than doing nothing!
Further Reading:
Learning Points
When initially history and information is light remember to clarify when more information is available.
Remember to use closed loop communication to confirm tasks are understood.
Consider utilising staff in their extended roles if they have the skills – this may allow you as team leader to step back.
Positive Feedback
Roles pre-assigned.
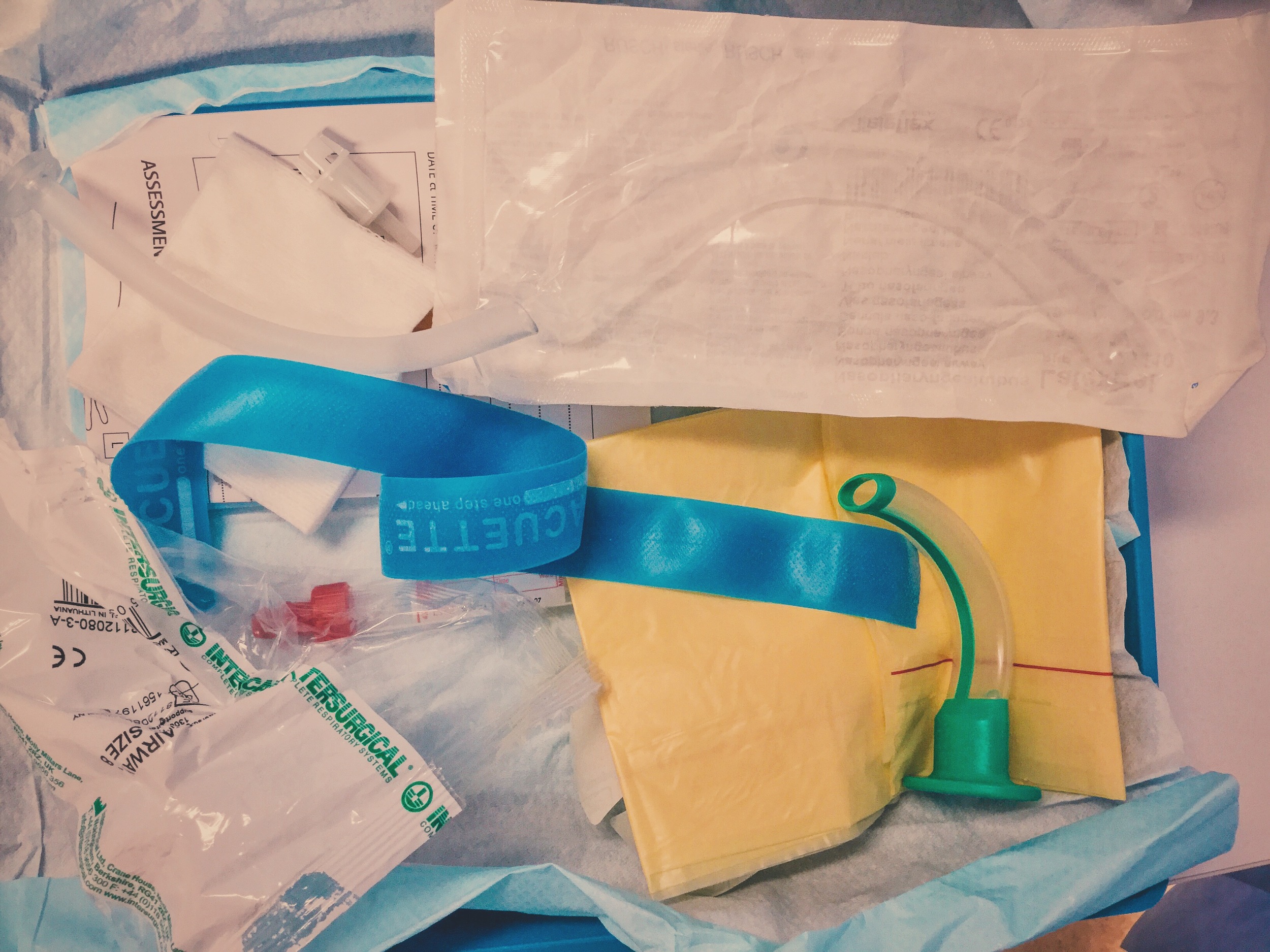
Good use of pre-alert time to prepare.
Correct management of seizure.