#SimBlog: Hypothermic Cardiac Arrest
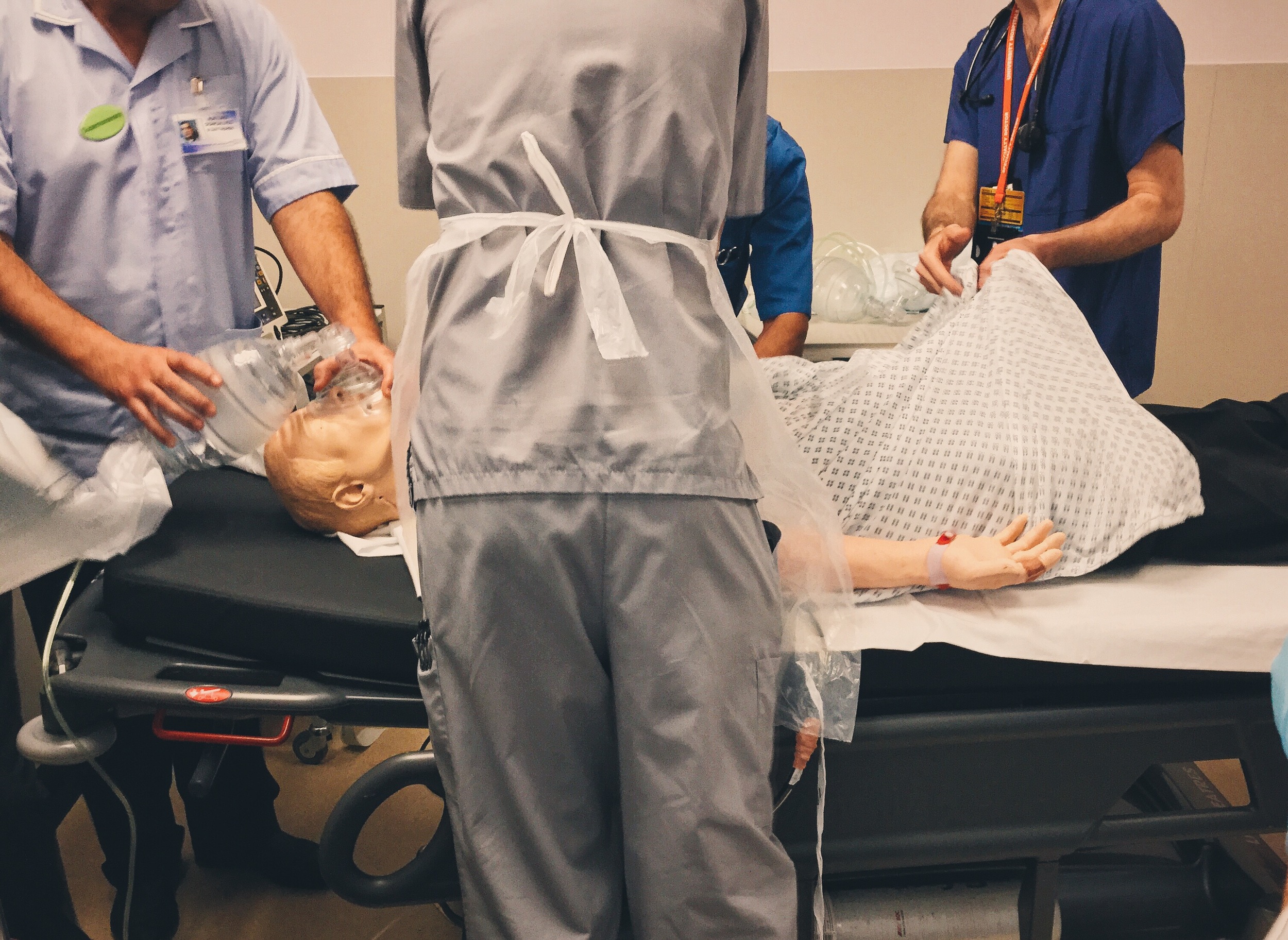
““Approx. 30 y/o male - found face down in a river. 45 mins of pre-hospital ALS and he has remained in asystole.””
Clinical findings
Unresponsive and in cardiac arrest
No airway interventions
Hypothermic: 32°C with tympanic thermometer
Why we simulated?
With colder weather hypothermia secondary to exposure is more likely to be seen. In the context of cardiac arrest it can present particular challenges. Discussion over the expression "they are not dead until they are warm and dead" should perhaps be expanded to include: "are they dead because they are cold or cold because they are dead?"
Remember also that hypothermia is a special circumstance and the ALS algorithm should be modified.
When presented with a no win situation, particularly in younger patients it can be very difficult to make decisions about stopping resuscitation and understanding prognostic factors is important for decision making.
Factors associated with improved survival are (Malhotra 2013):
Early BLS/CPR
Shockable Rhythms (and early defibrillation)
ROSC prior to arrival at hospital
Equally important is understanding the thoughts of other members of the team as some may not be ready to stop. Discussion around this is vital either during Resus or in a formal debrief after.
Finally it should also be stressed that if family are present the decision to stop needs to be communicated to them and it is a process they may wish to participate in.
Further Reading:
- #EM3: Lightning Learning – Hypothermia
- #EM3: Lightning Learning – Reversible Causes of Cardiac Arrest
- Cliff Reid at SMACC Gold – When Should Resuscitation Stop
- Roger Harris with a follow up at SMACC US – When to Stop Resuscitation
- RCEM Learning – Cardiac Arrest in Special Circs Hypothermia
Learning outcomes
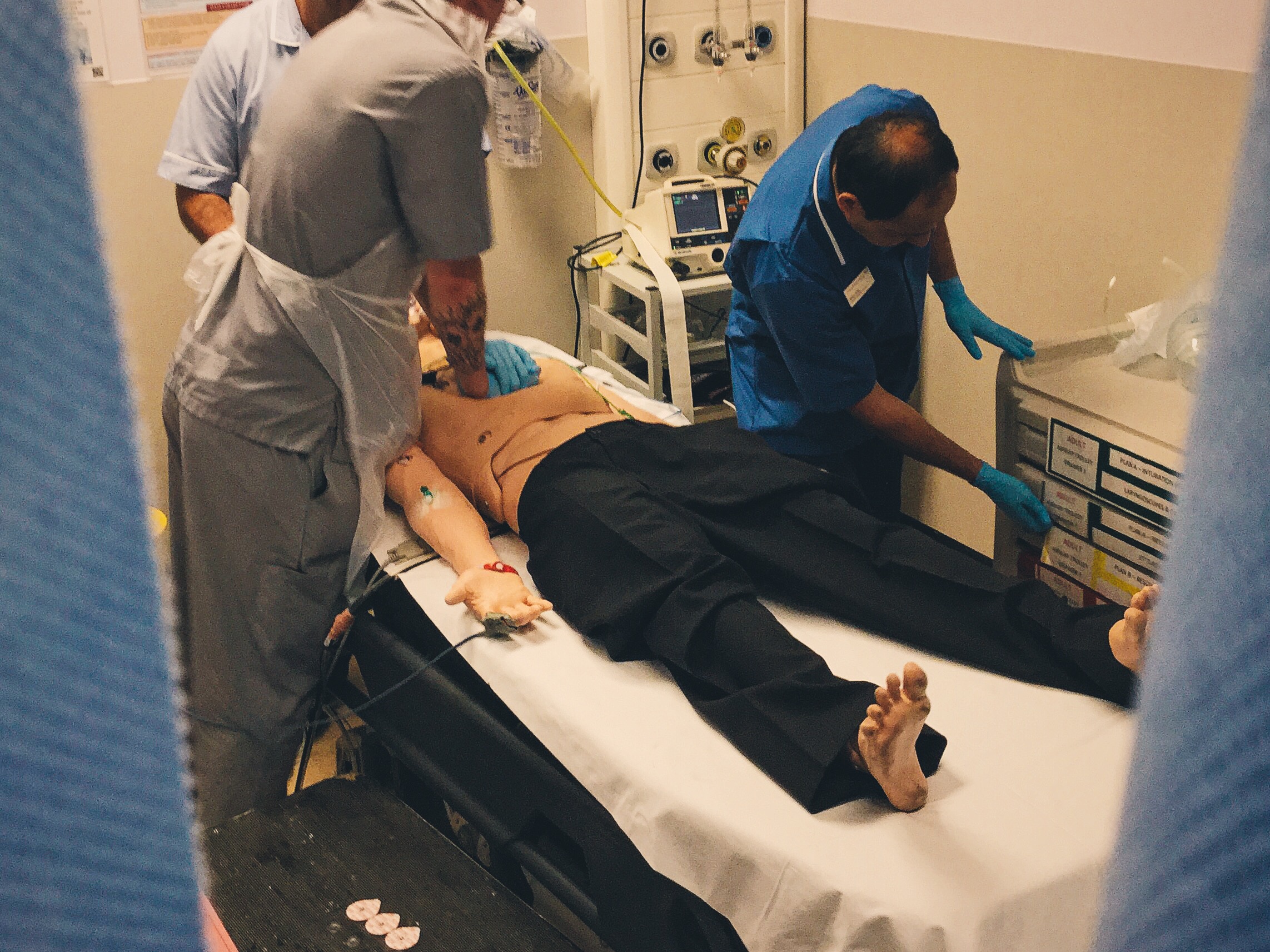
Without a definitive airway the ratio of compression to ventilation is 30:2
Consider drownings as trauma if the mechanism is unknown. This should include c-spine immobilisation.
"Historical clinical signs of poor neurological progress, including absent pupillary and motor reactions, are likely to require a prolonged period of at least 72 h to be reliable" (Temple 2012).
Positive feedback
Good allocation of roles and leader.
Team members verbalised when they were unable to perform tasks.
Considered the use of an automated CPR device (LUCAS in our trust) for prolonged resuscitation.
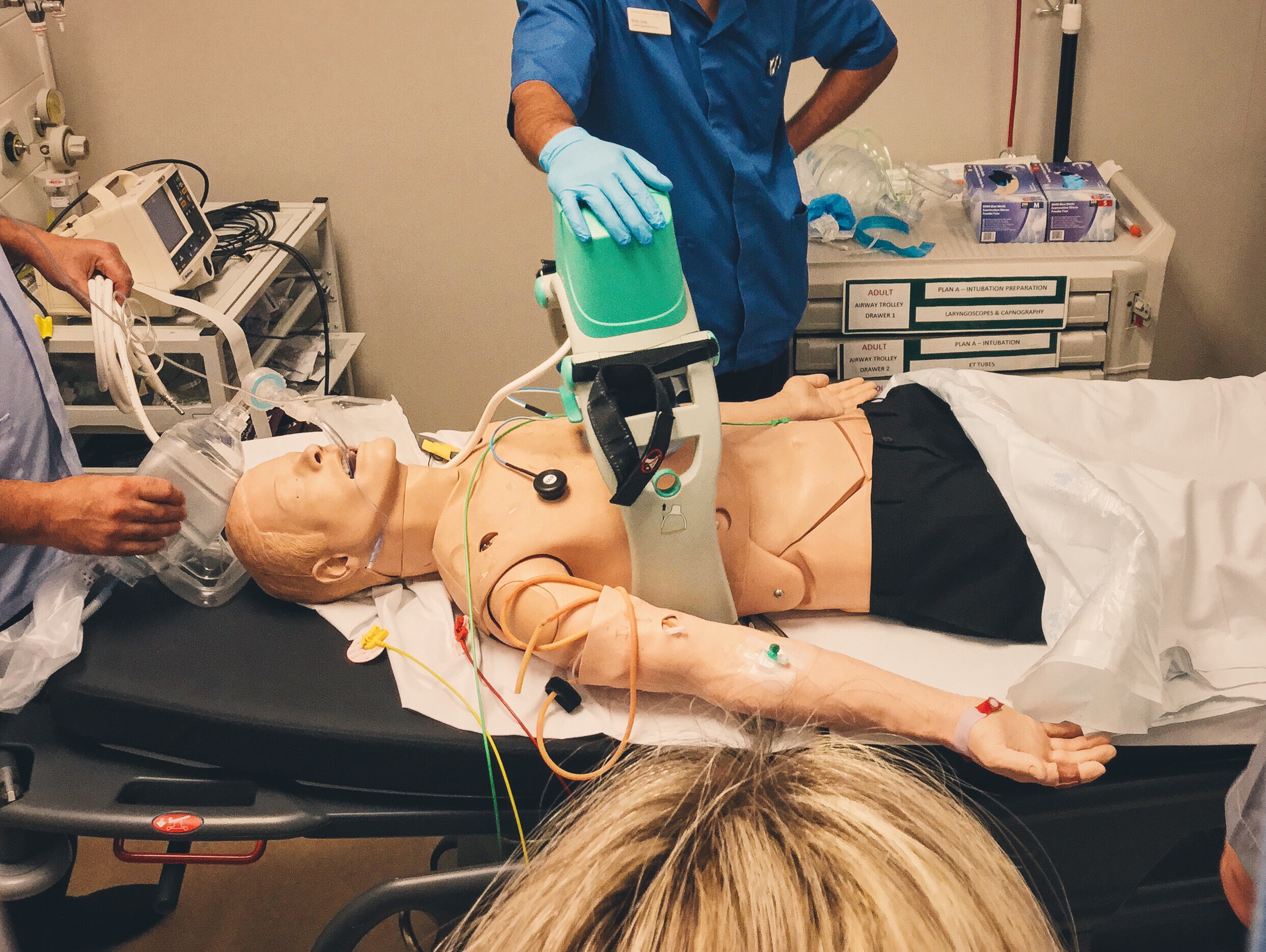
A guide on how to use a LUCAS™ device
References:
- A Molhotra, R. Rahkit Improving the UK’s performance on survival after cardiac arrest, BMJ 2013;347:f4800
- A.Temple, R. Porter, Predicting neurological outcome and survival after cardiac arrest. Contin Educ Anaesth Crit Care Pain (2012)doi: 10.1093/bjaceaccp/mks029