#SimBlog: Hypertensive Emergency
““A 78-year-old man feeling non-specifically unwell for a few days. 1 day of headaches and intermittently confused.””
Observations
A – Patent, self-maintaining
B – RR 18, SpO2 97% in air
C – HR 80, BP 214/128
D – GCS 15/15
E – Temp 37.1°C, BM 7.6
Clinical Findings
Intermittently confused
Vomiting
Severe hypertension
Why We Simulated
Hypertensive emergencies are defined as large elevations in Systolic or Diastolic Blood Pressure (>180 mmHg or >120 mmHg, respectively) associated with impending or progressive Organ Damage – ESH/ESC Guidelines for the Management of Arterial Hypertension 2013.
Locally our University Hospitals of Leicester Hypertensive Emergencies Guideline classifies a BP of >220/120mmHg as a hypertensive emergency.
Many of our patients who present to the Emergency Department (ED) may have elevated blood pressures recorded during their visit. This can be due to a number of reasons including pain, anxiety, missing their normal anti-hypertensive medications and "white coat hypertension".
Occasionally we see patients with blood pressure readings that fit the definition of severe hypertension, even so most patients will not require immediate treatment in the ED or admission to hospital for this reason alone.
So who can we safely send home and who needs more urgent treatment? The concern is not so much with the absolute numbers of the blood pressure readings but the effects of severe hypertension on the rest of the body. Patients with severe hypertension but no organ damage are often considered to be hypertensive urgencies rather than emergencies. They will require commencement of oral anti-hypertensive agents or alteration of existing regimen but can usually be discharged home with appropriate follow-up.
Hypertensive Emergencies
Patients who have severe hypertension alongside evidence of end organ damage are treated as hypertensive emergencies. Left untreated irreversible organ damage can occur within hours.
Organ damage can include:
Encephalopathy
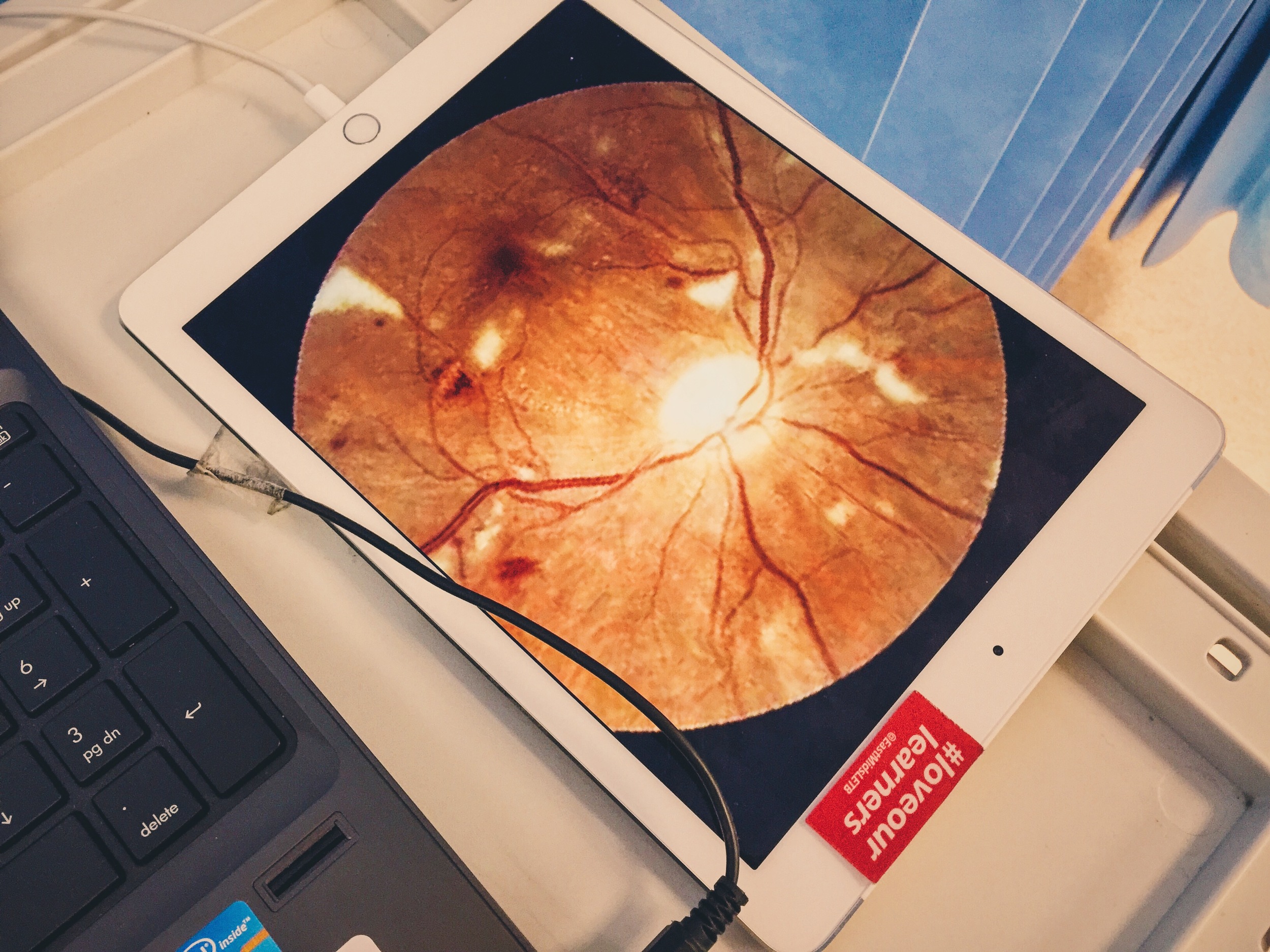
Grade III (retinal haemorrhages, exudates, cotton wool spots and retinal oedema) or Grade IV (papilloedema) retinopathy
Renal failure
Acute Coronary Ischaemia
LV failure
Aortic dissection (Recently highlighted in an RCEM Safety Alert)
Eclampsia (see our Previous Sim)
Hypertensive emergencies will usually require intravenous anti-hypertensive therapy aiming for a 25% reduction in blood pressure over 1-4 hours.
Patients with severe hypertension and retinal changes only (Accelerated hypertension) can often be managed with oral therapy such as a long acting calcium channel blocker aiming to reduce diastolic BP to 100mmHg over 24 hours.
References:
- ESH/ESC Guidelines 2013 – Management of Arterial Hypertension
- American Heart Association – Hypertensive Crises
- American Academy of Opthalmology: Eye Wiki – Hypertensive Retinopathy
- #EM3: Lightning Learning – Hypertensive Crises
Learning Outcomes
Features of hypertensive crises/emergencies
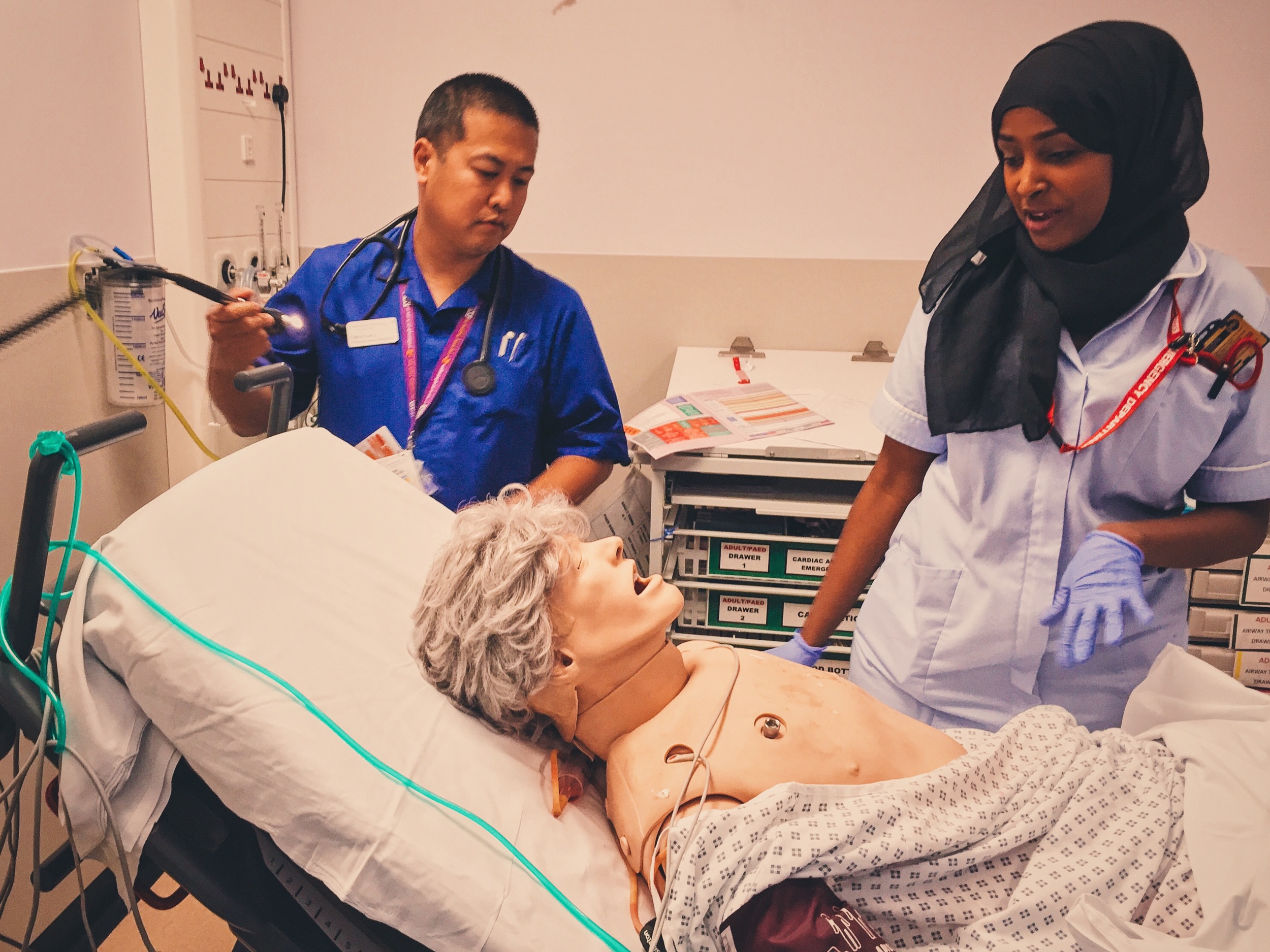
How sharing mental model can help with team dynamics
Ensure all team members utilised effectively
Positive Feedback
Good communication with patient
Sought senior help appropriately
Summarised what had happened so far