Suspected SAH: Do we still need the needle?
Background
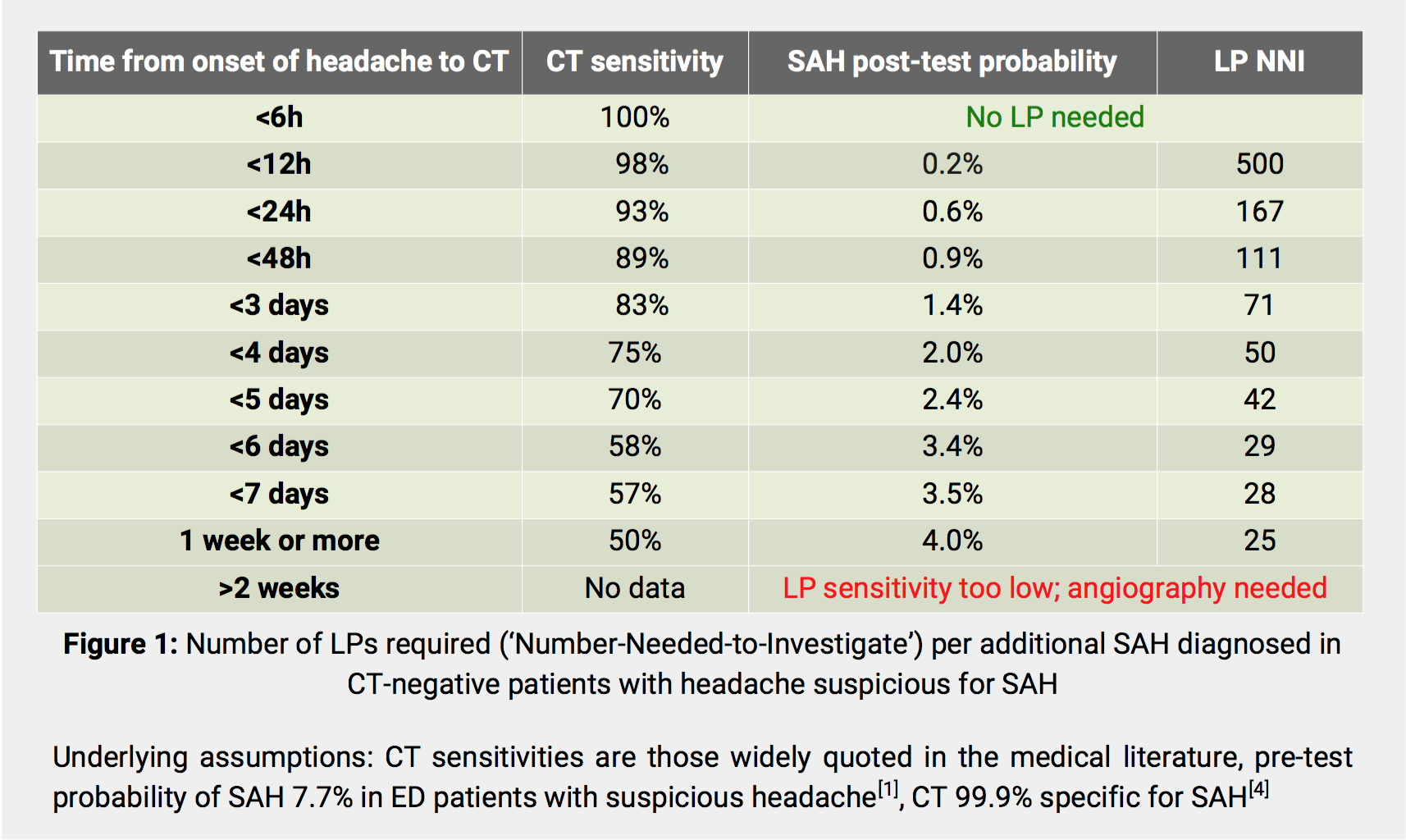
There is growing evidence that, due to advances in technology, early computed tomography of the head (CTH) can now reliably exclude subarachnoid haemorrhage (SAH) in neurologically intact people[1,2]. Despite this, current guidelines still demand that all CTH-negative patients undergo lumbar puncture (LP) to detect any remaining occult SAH[3]. Bayesian analysis reveals that, for every additional SAH identified by LP, potentially hundreds of patients are subjected to the risks of LP[4]. Of note, SAH detected by LP only is often non-aneurysmal and not requiring treatment[5]. We aimed to develop a clinical decision rule (CDR) that identifies patients at low risk of occult aneurysmal SAH in whom LP might be safely omitted.
Methodology
We devised the following candidate CDR: In neurologically intact patients with suspected SAH and negative CTH, LP is mandatory only if one or more of the following apply: Haematocrit less than 0.3, SAH high-risk factor present (defined as transient loss of consciousness, neck stiffness, diplopia, seizure, known unruptured intracranial aneurysm, history of intracranial aneurysm in at least one 1st-degree relative, previous SAH, family history of SAH, autosomal dominant polycystic kidney disease, Ehlers-Danlos syndrome type IV, fibromuscular dysplasia or pseudoxanthoma elasticum) or interval between headache onset and CTH greater than 48h. We chose the 48h cut-off point because the probability of a positive LP within that timeframe is less than 1% (see Figure 1) - a level of risk known to be acceptable to patients in relation to negative outcomes from a range of diseases and treatments.
Next, we reviewed all cerebrospinal fluid (CSF) samples analysed for bilirubin at our institution between Feb 2012 and Jan 2015. Patients with ruptured aneurysms in those with a positive or equivocal bilirubin spectrophotometry result were identified from their medical records. In addition, we searched our radiology information system (RIS) for ruptured intracranial aneurysms and identified those that had only been detected on repeated imaging. This was done in an effort to overcome a real-world limitation of our study arising from the fact that not every CTH-negative patient had actually undergone the LP mandated by current guidance. To maximize our chances of identifying any potentially remaining cases of aneurysmal SAH, we also scrutinised the Trust’s governance systems for complaints, incidents, claims and inquests relating to such patients.
The case histories of all patients with aneurysmal SAH as identified by the above method were analysed against our candidate CDR.
Results
712 CSF samples had been analysed for bilirubin during the study period. Angiography had confirmed aneurysmal SAH In 4 patients (see Figure 2). This indicates that in our Trust 178 LPs are currently performed for every additional aneurysmal SAH detected.
Three further ruptured intracranial aneurysms were identified from the RIS. No further cases came to light during our governance systems review.
Our candidate CDR correctly predicted the need for LP in all 7 patients with initial negative CTH who had aneurysmal SAH (see Figure 3).
Conclusion
Our findings suggest that a clinical decision rule (see Figure 4) can identify CTH-negative patients at risk of occult aneurysmal SAH. Since omission of LP is at variance with current guidelines, decisions to do so should at present be taken jointly with patients.
If validated, our findings could lead to a significant reduction in the number of patients requiring ‘the needle’.
References
- PerryJJ, StiellIG, SivilottiML et al. Sensitivity of computed tomography performed within six hours of onset of headache for diagnosis of subarachnoid haemorrhage: prospective cohort study. BMJ 2011;343:4277-87.
- BlokKM, RinkelGJE, MajoieCBLM et al. CT within 6 hours of headache onset to rule out subarachnoid hemorrhage in nonacademic hospitals. Neurology 2015;84:1927–32.
- Intercollegiate Stroke Working Party. National clinical guideline for stroke. 4th edn. London: Royal College of Physician, 2012.
- CoatsTJ and LoffhagenR. Diagnosis of SAH following a negative computed tomography for acute headache: A Bayesian analysis. EurJEM2006;13:80-3.
- HorstmanP, LinnFHH, VoorbijHAM et al. Chance of aneurysm in patients suspected of SAH who have a ‘negative’ CT scan but a ‘positive’ lumbar puncture. JNeurol 2012;259:649–52.