
Based at the University Hospitals of Leicester, we serve the educational needs of healthcare practitioners in Acute & Emergency Medicine across the East Midlands, UK

Based at the University Hospitals of Leicester, we serve the educational needs of healthcare practitioners in Acute & Emergency Medicine across the East Midlands, UK
Mrs Anne Faul
D.O.B. 16/8/1937
38 Marrow Drive
Bonebridge
LE7 9XL
Mrs Anne Faul is brought to the Emergency Department of XYZ NHS Trust by ambulance.
She presented with ?# NOF, ?#ribs, confusion & ?UTI; her last set of obs. were as follows: GCS 14, BP 189/96, HR 68, RR 26, temp 35.8°C; prioritised as category 2. She had received 2.5mg intravenous Morphine from the paramedics en route.
Ambulance call out was at 0845; on scene 0915; left scene at 0945; hospital at 1030.
Anne was 78 years of age, previously fit and well, and was on Ramipril 5mg/ Bisoprolol 2.5 mg and Paracetamol as needed for back pain. The next of kin was a niece, Sheila Hancock, who lived 30 mins away. That morning, Anne did not respond to repeated calls and door knocks from her caring neighbour at 0800 who found uncollected milk at the door – something Anne normally collected at 0715 every morning.
Hearing groaning and crying sounds, the neighbour, John, contacted the police who came and broke into the house. She was lying on the floor near the toilet and could not move because of hip pain. The ambulance was called and they collected her for the hospital. The bed seemed slept in and Anne was found incontinent of urine. No one knew when she fell. She lived in a bungalow and had a previous history of falls and a wrist fracture 9 months ago.
She had no history of dementia and although used to drive before, had not done so since the last fall as she did not feel confident. Recently she had even restricted going out much and John helped with the shopping.
GCS 14, RR 28, BP 190/92; HR 62; temp 36.8°C. Triage category 3. IV access obtained and bloods taken for FBC/ U&E/ LFT/Bone profile/ near patient testing including lactate, Trop I, ECG & urine dip.
Treatment given: IV Paracetamol 1 gm. X-rays requested – right hip, pelvis & chest. Initial nurse assessment showed tenderness right hip and right axilla. Anne was taken straight to XR from assessment area.
Anne is seen by Dr Scott, ST3 in the ED. History/examination as obtained: Collapse?Cause; poor historian, lives alone, see ambulance documentation. On Ramipril/Bisoprolol. XR shows inter-trochanteric # right NOF; ?small haemothorax right; no head injury or neck tenderness, abdomen/pelvis/limbs NAD. Seems comfortable. Bloods/ECG – all fine. CT head requested. D/W Consultant in ED. Started on IV Augmentin for UTI and confusion. Referred to orthopaedics 1330.
Anne was admitted to the Orthopaedic ward and left the ED at 1430 hours. While on the ward, she received further analgesia – regular Paracetamol, Codeine and Ibuprofen. The chest injury was discussed with the anaesthetists and the radiologists. She had 2 broken ribs but no obvious flail segments. She was reviewed by the medical SpR and the anaesthetists and it was decided to optimise her pain relief, continue with the antibiotics. The CT head had movement artefact but did not show any obvious injuries. Her chest injuries are reviewed by the Surgical SpR and no further treatment is prescribed except for chest physio to commence after surgery.
Anne is taken to theatre and has a dynamic hip screw inserted under GA.
Slow progress with PT/OT support and no complications. The confusion clears after 3rd post-op day. Now also on Calcium/D3 and had her Bisoprolol reduced to 1.25mg. Appetite/bowels – good. UTI – asymptomatic and antibiotics stopped after day 5. Anne not felt to have made good enough progress to be discharged home and is felt she would benefit from a short period in rehab.
Taken to community hospital for rehab.
Key words: fall, mechanism, fragility fractures, osteoporosis, trauma, head injury, hip fracture, CT scanning, pain assessment/management
Mrs Delilah Rheim
D.O.B. 6/12/1922
26 The Conifers
Befuddleridge
LE67 2TD
1st December call out 0800; at scene 0830; left scene 0915; arrived at ED 0945.
Found lying on the rug near the toilet, confused. Tender abdomen. Neighbour knocked on door. Key in key-safe. Bed not slept in. 94 year, widow. On Aspirin only.
SaO2 94% on air, Pulse 66, BP 156/82, RR 16, GCS 14/15 (M6 V4 E4), temperature 35.4°C.
1000. Difficult to assess. Not speaking much. Poor historian. No obvious injuries. Has external head trauma but moving neck. Chest crackles in both bases, limbs NAD, abdomen – ?palpable bladder – bladder scan shows 898 mls. Lives alone. Neighbour goes in daily – says Mrs R is normally fit and well, is a widow (husband was American) with no children or other family. Rest of history as before.
Plan: FBC, U&E, CK, CRP, CXR, catheterise and urine dip, IV meropenem, 0.9% saline 500 mls over 1 hr, CT head, admit to medicine. Hb 89, MCV 79, WCC 16.9, platelets 411, CK 2000, CRP 66, Urea 18.1, Cr 116, eGFR 40, CXR – cardiomegaly/patchy consolidation right base.
Admitted 1600. Confused with AMT 4/10. CT head shows mild small vessel disease. Examination findings – all normal. Catheter in situ. Urine dip – proteins, nitrate -ve, leucocytes +ve; sent for culture.
Plan: continue antibiotics; monitor renal functions, assessment of mobility. Admit to base ward.
Undergoes CGA. Repeat physical examination including PR – constipation.
Also, from GP, on regular Co-codamol 2 tabs QDS for knee pains. Opiates stopped. Catheters removed. Aspirin stopped. Discharged home after 3 days on Movicol and Iron tablets with OD care.
Ethel was an 84 year old lady who had been treated at her nursing home by her GP for increasing breathlessness over about a week or so. The nursing home staff were worried about her as she did not seem to be improving despite oral antibiotics. She was still breathless and just not her usual self. Although she had advanced dementia, requiring help with all activities of daily living, she was more drowsy and requiring more help than usual, for example with eating and drinking.
The nursing home called the surgery at 4pm, but the duty doctor was already booked up and so they were advised to send Ethel into the ED for further assessment. The ambulance crew arrived at about 5pm, and found her to be drowsy and uncommunicative. The initial assessment revealed GCS 13, pulse 104, BP 90/50, SaO2 87%, respiratory rate 28, chest clear, abdomen soft. Oxygen was administered, along with iv fluids and she was conveyed to hospital.
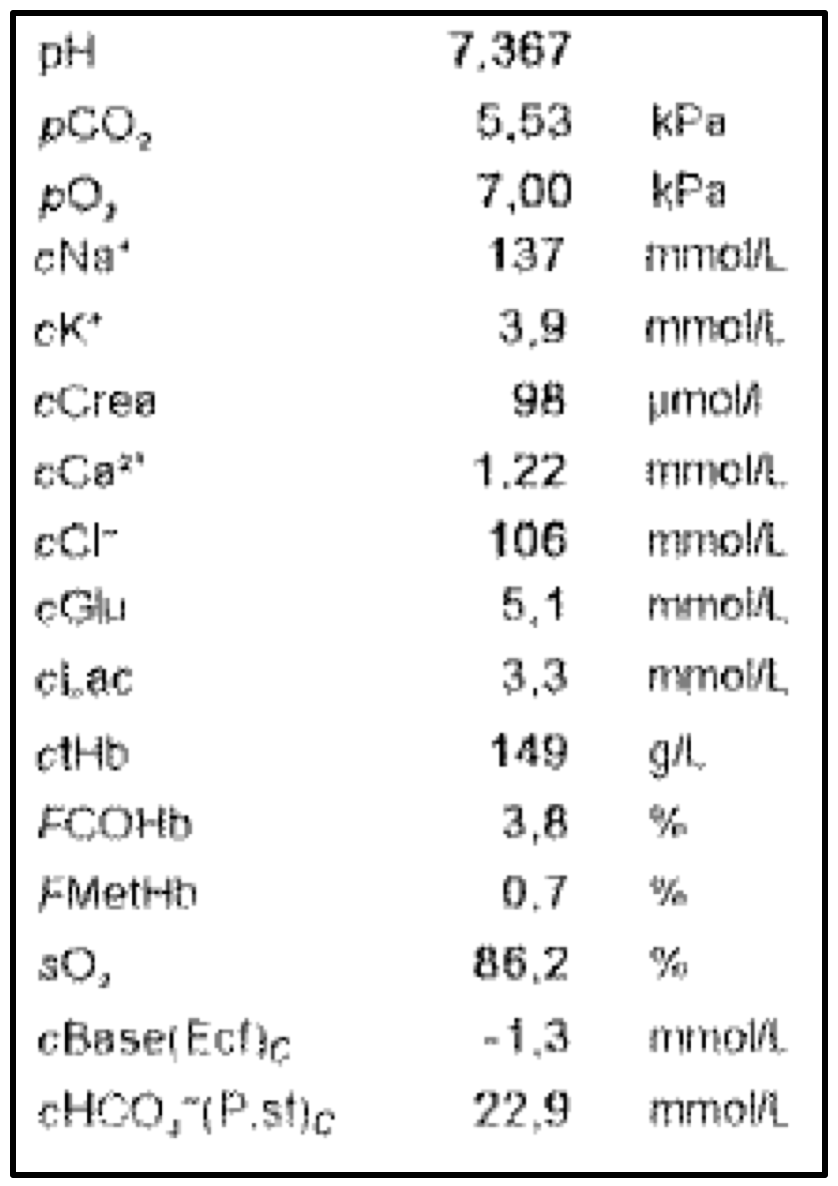
In assessment bay, sepsis was diagnosed, iv Meropenem started, fluids continued and a Blood gases showed:
She was referred to the Acute Frailty Unit, where she arrived at 1am. Her oxygen levels had improved with 28% oxygen which she was keeping on – saturations now 94%.
Blood pressure had improved to 110 systolic, but pulse still around 100; she remained drowsy and it proved difficult to elicit additional information from her. The assessing doctor called the nursing home, but the duty nurse was banking and did not know Ethel very well. She advised the doctor to read the care plan that was with her. The care plan described Ethel’s deterioration over recent months, to a point where she was fully dependant, bed-bound, doubly incontinence, but still usually able to eat with prompting.
She was unable to make any high level choices. Although there was a DNACPR order in place, there was little additional information about her wishes and preferences, although her daughter was mentioned as next of kin.
By the time of the consultant ward round at about 8.30am, Ethel was little changed – essentially stable. He bloods showed little additional information other than a WCC of 11.4 and a CRP of 24. The antibiotics were continued and she was transferred to a base ward.

Chest X-ray
Ethel died in hospital a few days later. Her daughter was with her when she died. Ethel was comfortable, well cared for, pain free. Her daughter expressed her thanks to the team for the care they had provided. A post mortem was not undertaken and the death certificate was issued as 1a Community acquired pneumonia, 2 dementia.
Questions:
Was this a good end of life experience for Ethel?
What could have been done differently in the nursing home, by the ambulance crew, in the ED or in the frailty unit?
Do you agree with the death certificate?
How much of this was predictable?
Jack is a 90 year old man who attended the emergency department following a fall which resulted in a head injury. He had fallen whilst walking back from the shop; he was carrying two bags at the time. He remembered feeling ‘drained’ and described a vague wooziness. He was also able to recall trying to navigate between some fencing and a parked van, losing his balance and trying to break the fall using his arms, but was hampered by the bags he was carrying.
He sustained a significant laceration to his forehead. The assessment doctor requested a CT scan, which showed no significant changes. The wound required suturing. Jack was unable to recall how he had managed to hit his head. Bloods were unremarkable. As it was late in the evening, he was transferred to the Emergency Frailty Unit for an overnight stay and MDT review in the morning.

After a reasonably restful night, further review the next day revealed several additional problems – urinary frequency and incontinence, for which he was taking Tamsulosin (his only prescribed medication), clinical evidence of sarcopaenia and poor vision in his left eye, though to be cataract related.
He was seen by the physiotherapist, stood unaided and was able to walk to the bathroom and back without event. He lived in a bungalow and so there was no need for a stairs assessment. He denied any offer of additional support at home as he had good neighbours and family who were local and supportive. He was bright and cheery throughout all the assessments but was eager to return home.
It emerged that he had already been referred to the falls clinic in Melton, so later went home with that as follow up.
Questions:
Did Jack need to be admitted?
Did he need a CT head?
Did we deliver CGA?
Why did he fall?
Should we continue Tansulosin?
What can we do to prevent a future fall?