#MiniTeach: Warfarin & Head Injury
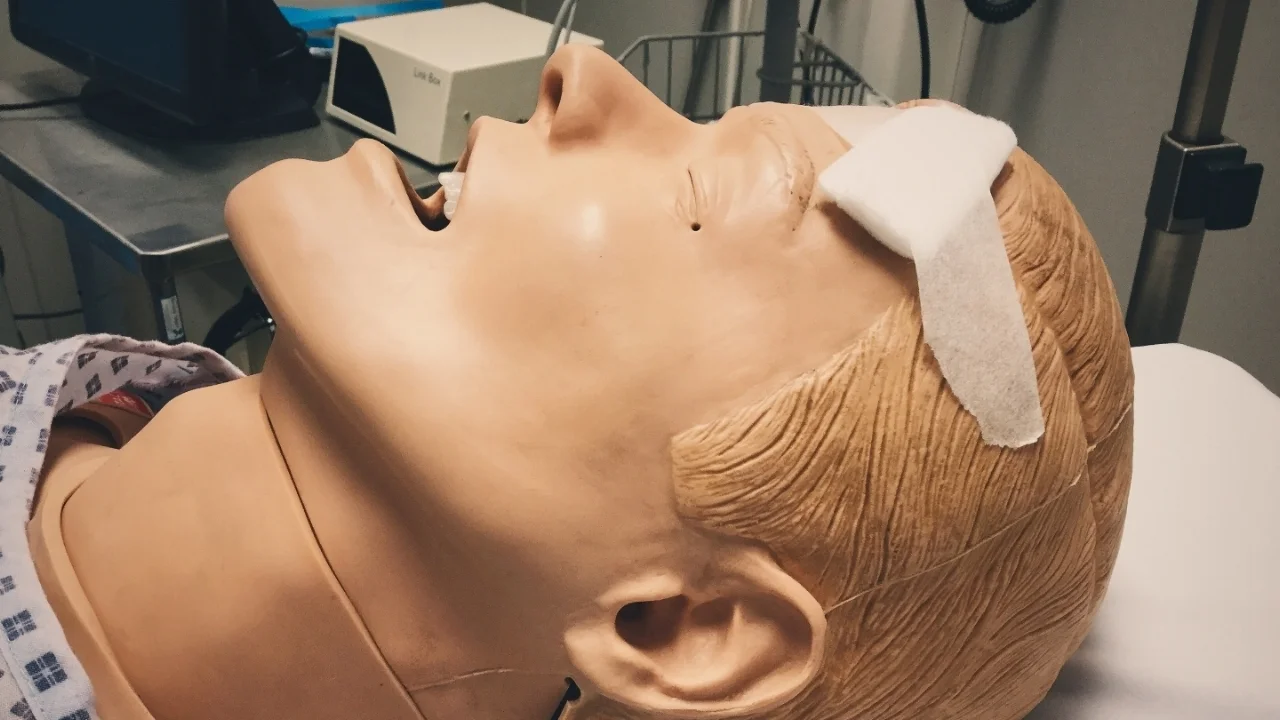
"An 81 year old man presents to the Emergency Department with a GCS of 3/15 having sustained a minor head injury two days previously."
He has atrial fibrillation and is on warfarin. ITU are called and he is transferred to CT, intubated and ventilated. The CT scan is attached. His INR is 3.4.
1. What does the CT scan show?
There is a large acute subdural with mass effect, midline shift, hydrocephalus and uncal herniation.
2. How does warfarin work?
Warfarin inhibits an enzyme called vitamin K epoxide reductase. This enzyme is responsible for recycling vitamin K and so warfarin limits the amount of active vitamin K available for blood coagulation.
Vitamin K is required for activating clotting factors II, VII, IX, X, Protein C, S and Z which are parts of the extrinsic pathway of coagulation, which is responsible for producing a thrombin burst.
3. What is INR and why is it used to monitor warfarin therapy?
Warfarin requires monitoring because it has a narrow therapeutic index and it has many interactions with other medications and foodstuffs.
INR stands for International Normalised ratio. To understand it, you have to understand how they process the blood in the lab.
When you take a coagulation sample for an INR, you put the sample in a bottle containing citrate. This binds calcium in the blood and stops it clotting. The proportion of blood to citrate needs to be fixed to give accurate results, hence why they can’t process an under-filled sample.
The sample is sent to the lab where it is centrifuged, which separates the blood cells from the plasma. Calcium is then added back into the plasma, which allows it to clot.
Tissue factor (factor III) is then added and the time for the blood to clot is measured.
Manufacturers produce tissue factors in batches, which have slightly different properties. To overcome the effects of these different properties and to give consistent results, a mathematical equation is done, which corrects the effects of these properties, giving the INR.
4. How would you reverse this man’s coagulation and what considerations do you need to take into account?
Guidelines for reversal for warfarin exist on the intranet. This man needs rapid, effective reversal and so giving prothrombin complex concentrate (PCC) and vitamin K should be the first line treatment.
PCC is derived from plasma and has the potential to rarely cause transmission of viruses and CJD.
There is an increased risk of thrombosis, so relative caution should be taken in a patient who has recently had a myocardial infarction or suffers from severe angina.
There is a small risk of allergy.
If the patient has capacity, you need to get informed consent as with most blood products.
To commence PCC, download the ‘PCC pack’ from the intranet and follow the instructions.
Only the haematology doctor on call can authorise its use as it is expensive. They will need to know the patient’s weight in order to give the correct dose, so obtain this before you make the call.
Now imagine the patient has presented two days earlier after his minor head injury. He reports falling down two stairs, hitting his head on the banister. There was no loss of consciousness, no amnesia and he walks into the department with a GCS of 15.
5. How would you now manage him?
You would need to perform a full assessment, looking for neurological function including GCS, pupils, gait and signs of vault or base of skull fracture (panda eyes, battle’s sign, CSF from ears or nose and haemotympanum – yes, that means looking in the ears).
If all of this proved normal, then according to the current NICE head injury guidelines a CT should be performed within 8 hours. Pragmatically this should probably happen in ED as it is trickier to arrange from the wards especially out of hours.
The question is - do you need to check the INR?
The NICE guidelines don’t give advice on this particular issue, which means that it sometimes isn’t considered as part of the work-up. Assessing the INR might enable you to better risk-assess the chances of him bleeding at a later stage and if necessary, consider reversal of warfarin now.
The British Journal of Haematology did issue guidelines on this aspect of head injury care in warfarinised patients in 2011 and suggest doing just this (see attached).
The patient may still be safe for discharge, but as always should go home with head injury advice given and explained to him.