#MiniTeach: Hot And Bothered
"A 7-month-old boy is brought in by his mum who reports he has a history of fever over the last 24 hours."
She feels he is more sleepy, is feeding less, and has a reduced number of wet nappies. He vomited once a couple of hours ago. His past medical history, birth history and family history are unremarkable. This is his first attendance to PED.
1. As the first person to assess him, what would you do?
This child needs to be assessed and treated in accordance with CG160 Feverish illness in children - NICE Guidance.
There is a NICE feverish illness in children pathway to help you.
Important point: Reported parental perception of a fever should be considered valid and taken seriously by healthcare professionals. Even if this chid was apyrexial at time of arrival to the department, the history of a temperature must be taken as fact.
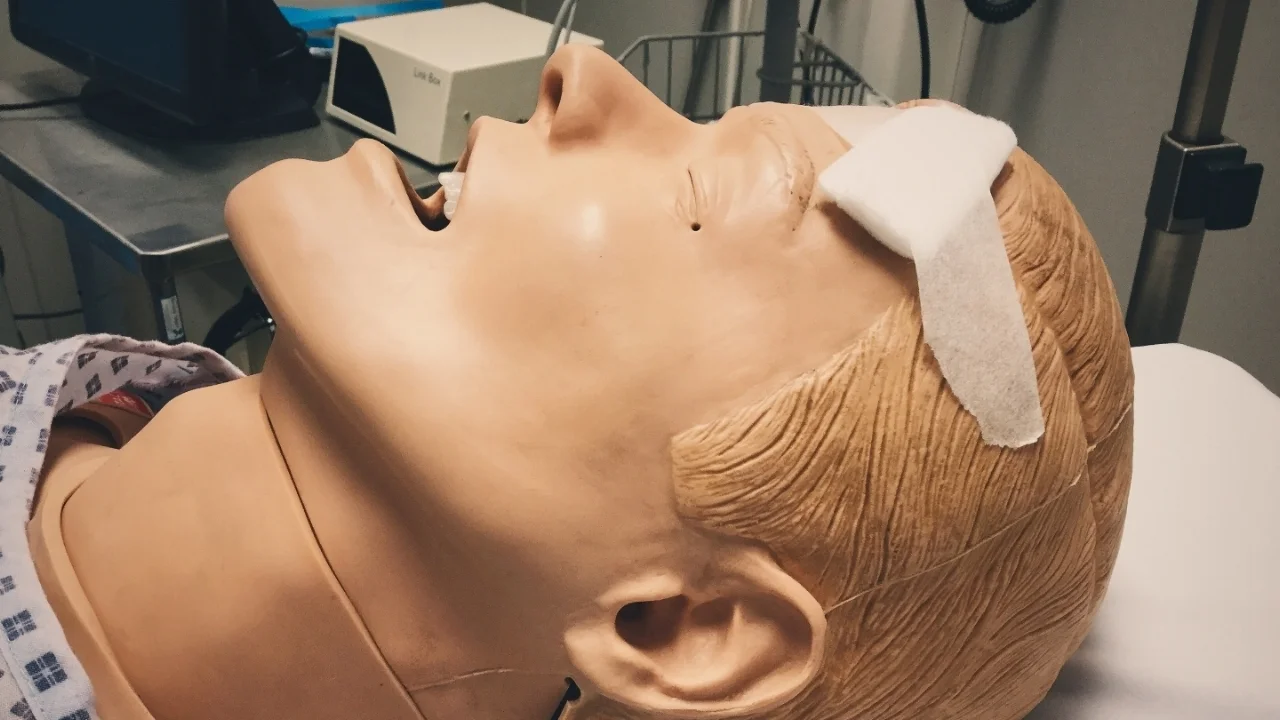
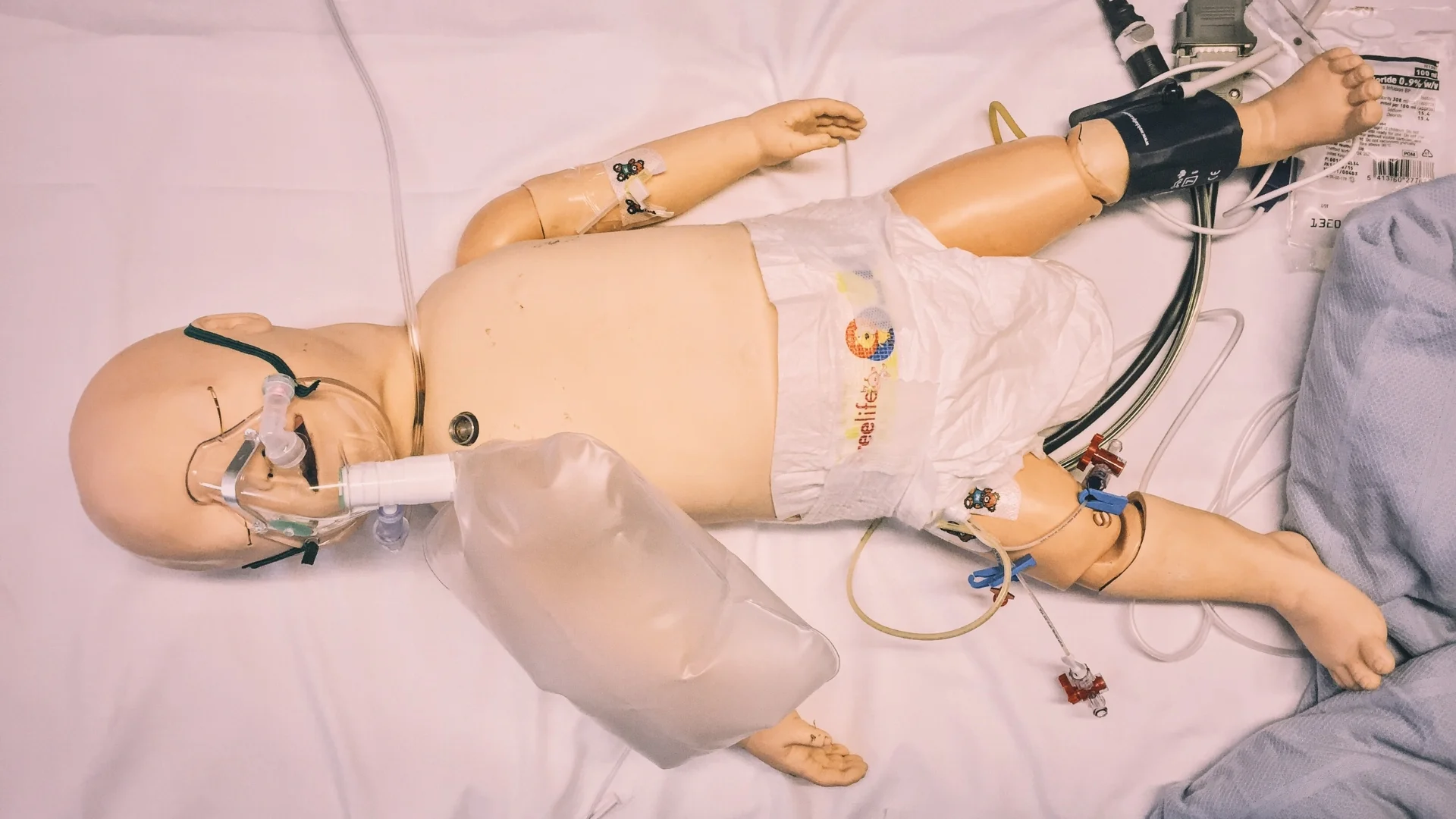
Undress him completely to identify life - threatening features (ie. A,B,C,D, E assessment).
Assess him to enable a Paediatric Observation Priority Score to be calculated (POPS -The Paediatric Observation Priority Score — University of ...) (pulse, respiratory rate, and temperature, related to his age, oxygen saturations, assessment of work of breathing, assessment of his level of alertness, your gut feeling and any other risk factors (e.g. oncology patient, congenital heart disease etc). The higher the score, the more concern should be held for the infant. If his score is elevated above 8, this infant may require resus.
Obtain a BM - if less than 3, follow the Paediatric Hypoglycaemic pathway (Intranet).
Give an antipyretic if the child is unsettled, liquid paracetamol should be the first agent if not given in the previous 4 hours.
If the infant appears well with a normal POPS score, encourage the Mum to feed the infant as normal, and to document what the infant manages to tolerate
Give the mother the equipment required to perform a clean catch urine sample (including advice regarding cleaning the infant first) and set her up for this.
On examining the infant he is pyrexial: Temp 38°C, a bit unsettled, Pulse of 190 bpm, RR 40 with no other abnormal examination findings, BM 4.2
2. What would you do next?
Firstly, assess the child for the presence or absence of symptoms and signs that can be used to predict the risk of serious illness using the NICE traffic light system for identifying risk of serious illness:( CG160 Feverish illness in children: support for education and learning: educational resource - traffic light table).
Important points:
Children with tachycardia are in at least an intermediate-risk group (AMBER) for serious illness.
“Reduced feeding in this infant” and “reduced urine output” put the infant in an "at least intermediate risk of serious infection (AMBER)" group – even if he “looks” well!
Assess the child for Symptoms and signs of specific illnesses. This includes obtaining a clean catch urine sample.
"Management by the non-paediatric" versus the "paediatric practitioner":
This may cause you some confusion as you may have little paediatric experience, but you are managing the child in a Paediatric Emergency Department. As a child with no underlying diagnosis, 3 possible AMBER signs and the provision of a Children's Assessment Unit, it would be prudent to ensure that the child has a period of time to ensure that the feeding pattern is assessed and the urine output can be assessed as adequate, plus further investigations to determine the cause.
This may not always be possible within PED due to time constraints and so referral to the paediatric team on CAU for assessment may be warranted.
NICE guidance for Management by paediatric specialists, recommends that, in addition to blood tests and urine, “a period of observation in hospital should be considered as part of the assessment to help differentiate non-serious from serious illness”.
Before you have decided where to send the patient, it appears the child has responded to the antipyretics given to him at assessment and his temperature and abnormal pulse and respiratory rate have returned to normal.
3. What should you do now?
In children aged 3 months or older with fever without apparent source, a period of observation in hospital (with or without investigations) should be considered as part of the assessment to help differentiate non-serious from serious illness.
Important point: Remember - this child may look "well" but is still at an intermediate risk of a serious infection!
4. If this child was 11 weeks old, would you do anything differently?
Yes - these are a very different clinical group, and the history of a temperature alone >38 in this age group immediately puts this infant in a High risk of serious infection RED group and necessitates its own clinical pathway. This will be a whole new mini teach - so watch this space!
In addition, look at the NICE pathway, and IMPORTANT POINT – all children under the age of 3 months MUST be discussed with a senior!