#MiniTeach: A Post Operative Problem
WARNING: this post pre-dates SEPSIS 3.0 & may refer to older definitions
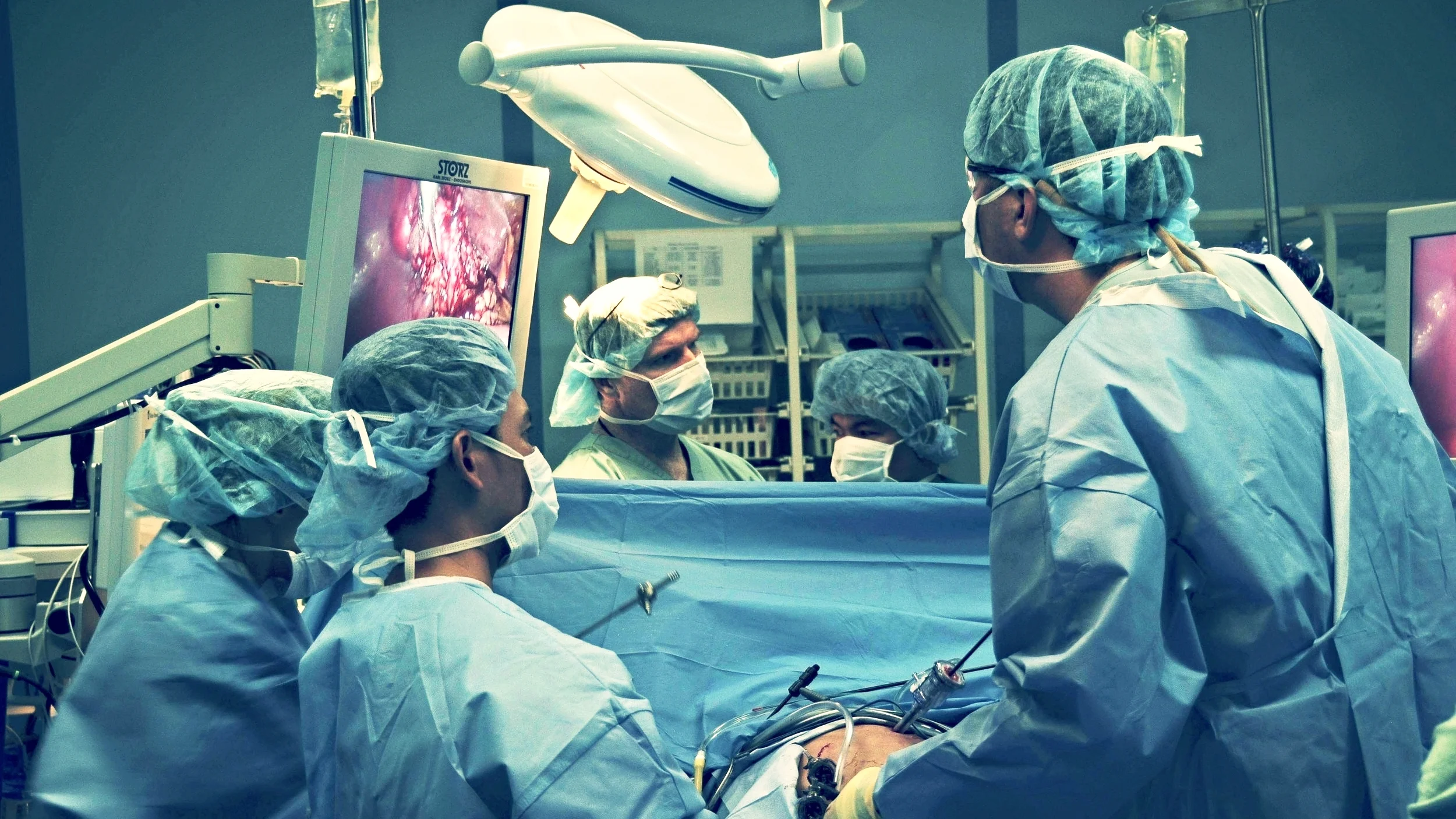
"A 58-year-old lady presents by ambulance to the ER. She was discharged the previous day having undergone day-case laparoscopic cholecystectomy."
She has noticed worsening abdominal pain since discharge. The paramedics have given her entonox and 250mls of normal saline via a cannula. Obs in the ambulance were: Pulse 106, BP 86/57, Temp 36.5°C, RR 26. She has been red-called to ER.
You decide to perform near-patient testing. Here are the results of the venous blood case and FBC:
pH: 7.315
pCO2: 4.62
pO2: 2.56
BE: -8.0
HCO3: 17.2
Na: 132
K: 4.1
Lac: 9.0
Urea: 7.6
Hb: 13.1
WCC: 3.5
Plat: 123
You also request a CXR:
1. As the assessing nurse in Resus, what further information will you seek at this time and what action will you take?
Has the patient had any analgesia apart from entonox in the prehospital setting?
Have they had any vomiting or diarrhoea? Has there been any bleeding? Have they been feeling feverish or had a temperature?
Do they have any other problems with their health? Are they allergic to anything?
Perform a full set of obs: Sats, pulse, BP, temperature, BM, GCS, RR. Calculate the EWS.
(It is very important not to estimate respiratory rate in these patients and to count it carefully. A raised respiratory rate is one of the most sensitive clinical indicators of critical illness).
Ascertain the patient’s pain score and ensure that further analgesia is offered if required. If the observations are not improved, ensure that the senior doctor in Resus is aware that you are concerned that the patient is unwell and gets seen quickly.
In you are able, obtain FBC, U+E, LFT, Amylase, G+S, Blood culture and near-patient testing. Ensure that the cannula is working, the fluids have gone through and query with the doctor whether they would like any more now.
2. As the advanced nurse Practitioner or junior doctor in Resus, what are you looking for in your focused history and examination?
You will be keen to ascertain why the patient had the surgery and who was the surgeon.
Get a full SQUITAS history regarding the pain: Site, Quality, Timing, Intensity, Alleviating and exacerbating factors, and associated Symptoms. (Vomiting, passing flatus, distension, bowels, bleeding, urine output). Any respiratory symptoms? Any cardiac symptoms?
Does the patient have any other medical problems? Is she diabetic? Were there any problems during or immediately after the operation? Is she on any medications? What analgesia was she discharged with?
ABCDE!
The examination will cover a general examination. How does she look? What is your gut telling you? Is she pale/clammy/in pain?
What is her abdomen like? Soft? Distended? Tender? Is there any rebound or guarding? Is there any rigidity? Are there bowel sounds? (Your patient is quite obese, so be aware that clinical signs may be less apparent).
3. What potential complications of laparoscopic surgery should you be thinking about?
Laparoscopic surgery can result commonly in wound infections and bleeding and bruising around the port sites, which is usually minor and would not result in severe pain.
More serious complications are perforation of intra-abdominal organs (anything from bowel to diaphragm), vascular injury leading to bleeding.
Specific to lap chole would be bile leakage, injury to the common bile duct.
Post cholecystecomty syndrome.
General surgical complications: DVT, anaesthetic risk, pneumonia etc.
http://www.medicalprotection.org/southafrica/casebook-may-2012/the-risks-of-laparoscopic-surgery
4. What do you think is going on with this patient? What is your management plan?
Clinically, the patient has SIRS – systemic inflammatory response syndrome. This is a whole body immune response, which frequently occurs in the presence of infection, in which case it indicates sepsis but can also occur in other insults such as burns, haemorrhage, pancreatitis etc.
A patient has SIRS when at least 2 out of 4 of the criteria are met:
Temp either <36 or >38
Pulse >90
RR>20 (see why getting that RR count right is so important?)
WCC <4 or >12
This patient has P 112, RR 26 and WCC 3.5, so she has 3 out of 4 of the SIRS criteria. Once you have identified SIRS, the question to ask is ‘what’s causing it?’.
The blood results show that the patient has a lactic acidosis and that their white cell count is low.
The exceptionally high lactate with the observations recorded tell you that the patient is sick. Even if she looks well from the end of the bed. The likelihood is that she has a serious post-operative complication, such as a perforation that is causing intra-abdominal sepsis.
Your management plan is to ensure that the patient has good IV access and to institute aggressive fluid resuscitation.
Insert a urinary catheter and measure urinary output on an hourly basis, ensure that the patient has appropriate analgesia.
Get a CXR – to check for signs of pneumonia or diaphragmatic perforation.
Don’t get an AXR – this is unlikely to be useful in this patient in altering management and we don’t want this sick lady to be waiting round in x-ray for hours.
Start the patient on the sepsis proforma and give the sepsis 6.
The patient’s CXR is included. As the ED registrar you decide to call the surgical registrar to review the patient in Resus. When you call the registrar, they advise you to get a CT abdomen and that they’ll review the patient afterwards.
5. What are your next steps?
You are worried about this patient and need to ensure that the surgical registrar has taken her abnormal physiology seriously.
Ensure that you have communicated the information effectively using RSVP and made the registrar aware that she has SIRS and a lactate of 9.
You are concerned that the patient may have a serious complication of laparoscopic surgery, such as perforation and you worry that a CT scan at this juncture may provide a false sense of reassurance as it may just show post-operative changes, even in the presence of a perforation.
You require the surgical registrar to come to resus to review the patient now. If the registrar refuses, you have a duty of care to your patient to call the surgical consultant on call.