#SimBlog: Time Critical Transfer
““A pre-alert is made for a 5-year-old boy who is screaming in pain complaining of a sudden onset headache. His GCS drops during assessment…””
Observations
A – Patent
B – RR 24, Sats 96%
C – HR 140, CRT 2 seconds, BP 110/80
D – BM 7, GCS 13/15 (E4 M5 V4)
E – Temp 36.8°C
Clinical Findings
No findings to suggest head injury
GCS drops to 8 during examination
Unequal pupils – right 5 mm and left 3 mm
Why We Simulated?
There are occasions when paediatric patients require emergency inter-hospital transfer in order to facilitate a life-saving intervention which is not readily available onsite and which cannot wait for stabilisation or retrieval. The commonest clinical scenario likely to require Time Critical Transfer from our hospital is that of a child with an expanding intracranial haemorrhage who requires immediate neurosurgical intervention at the nearest paediatric neurosurgical facility.
Coordinating the care and timely transfer of these children relies upon collaborative team working from the ED, Anaesthetics, Children’s Intensive Care, Ambulance Service and Radiology Departments.
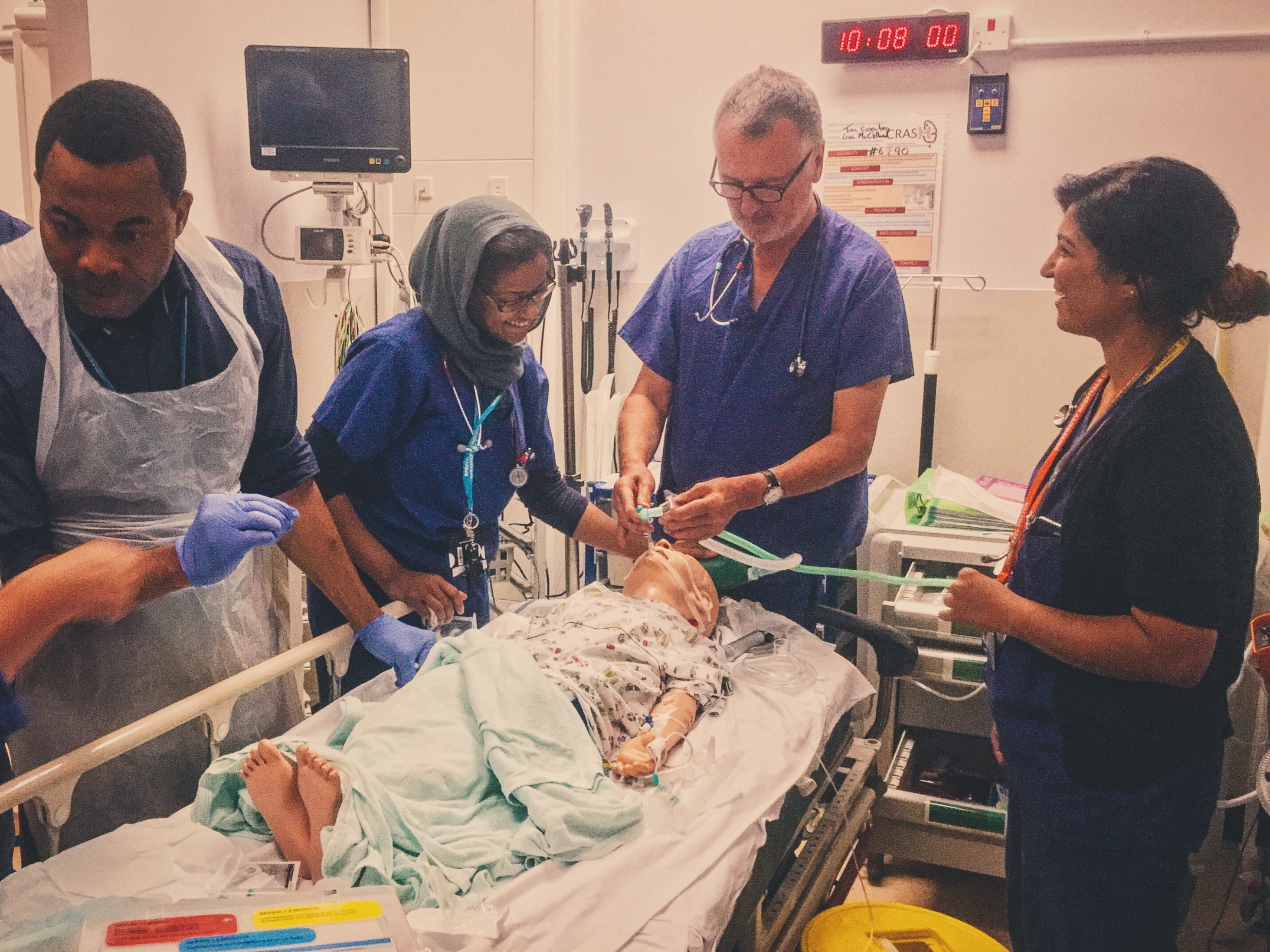
We ran a large scale interdepartmental paediatric simulation involving all these teams with special assistance from the Gaumard team who provided us with a wireless paediatric simulator. This enabled us to simulate the entire patient journey – starting with the pre alert to Resus from the paramedic crew on route to the ED and finishing with the patient loaded into the departing ambulance on the transfer trolley.
Our aim was to create a realistic scenario where these teams could gain experience working together whilst ensuring SWIFT and SAFE patient care in this pressurised situation.
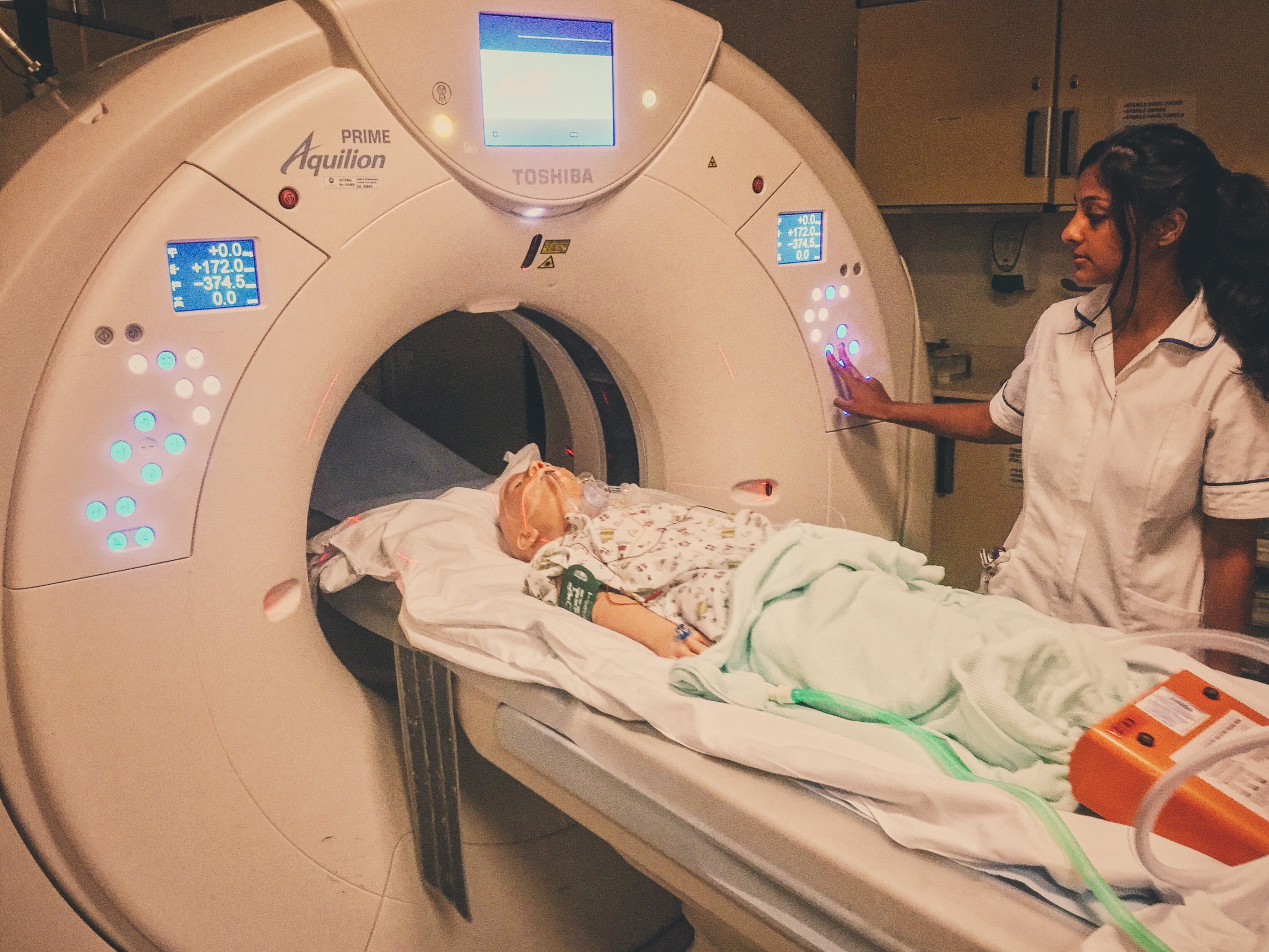
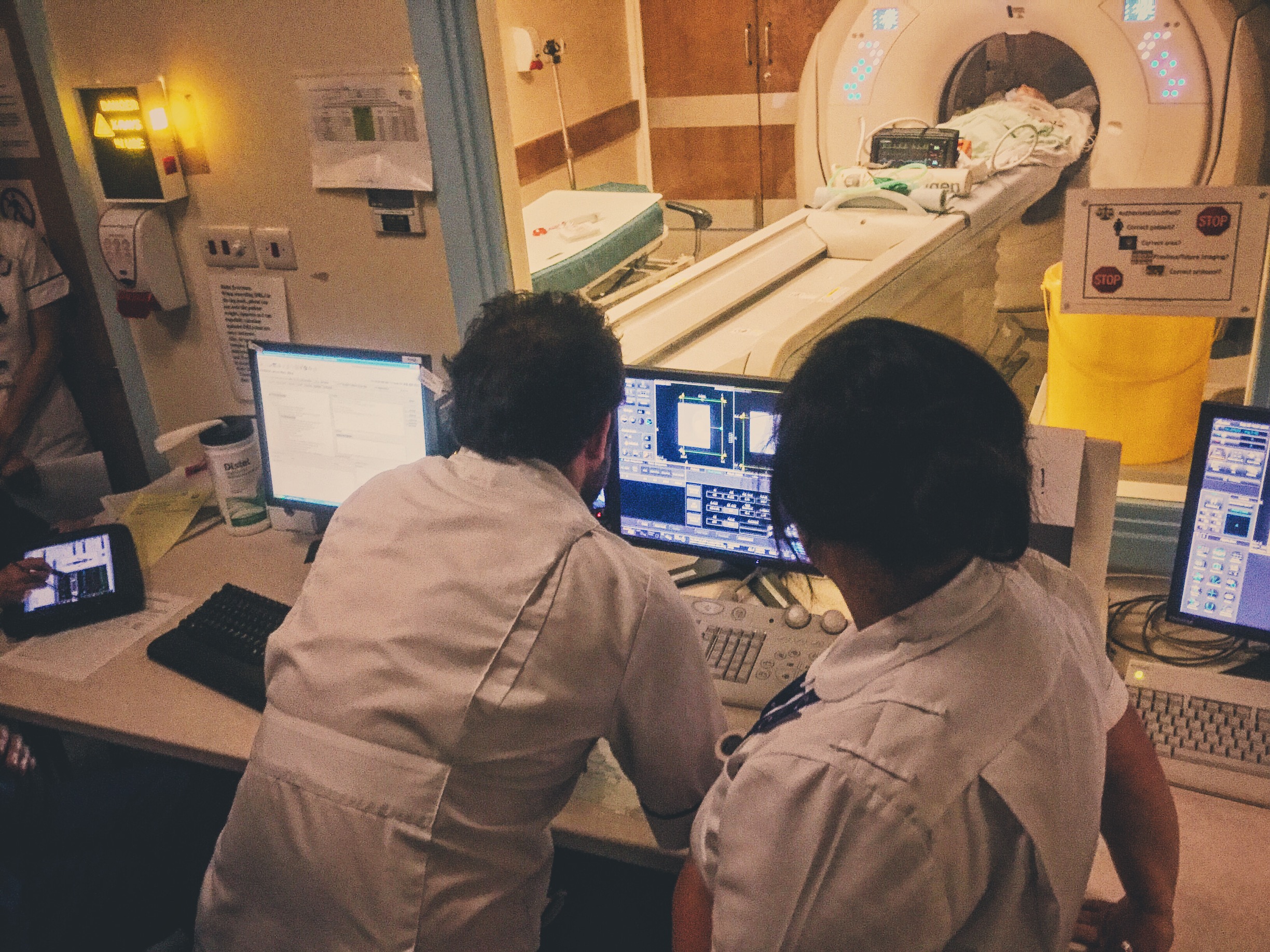
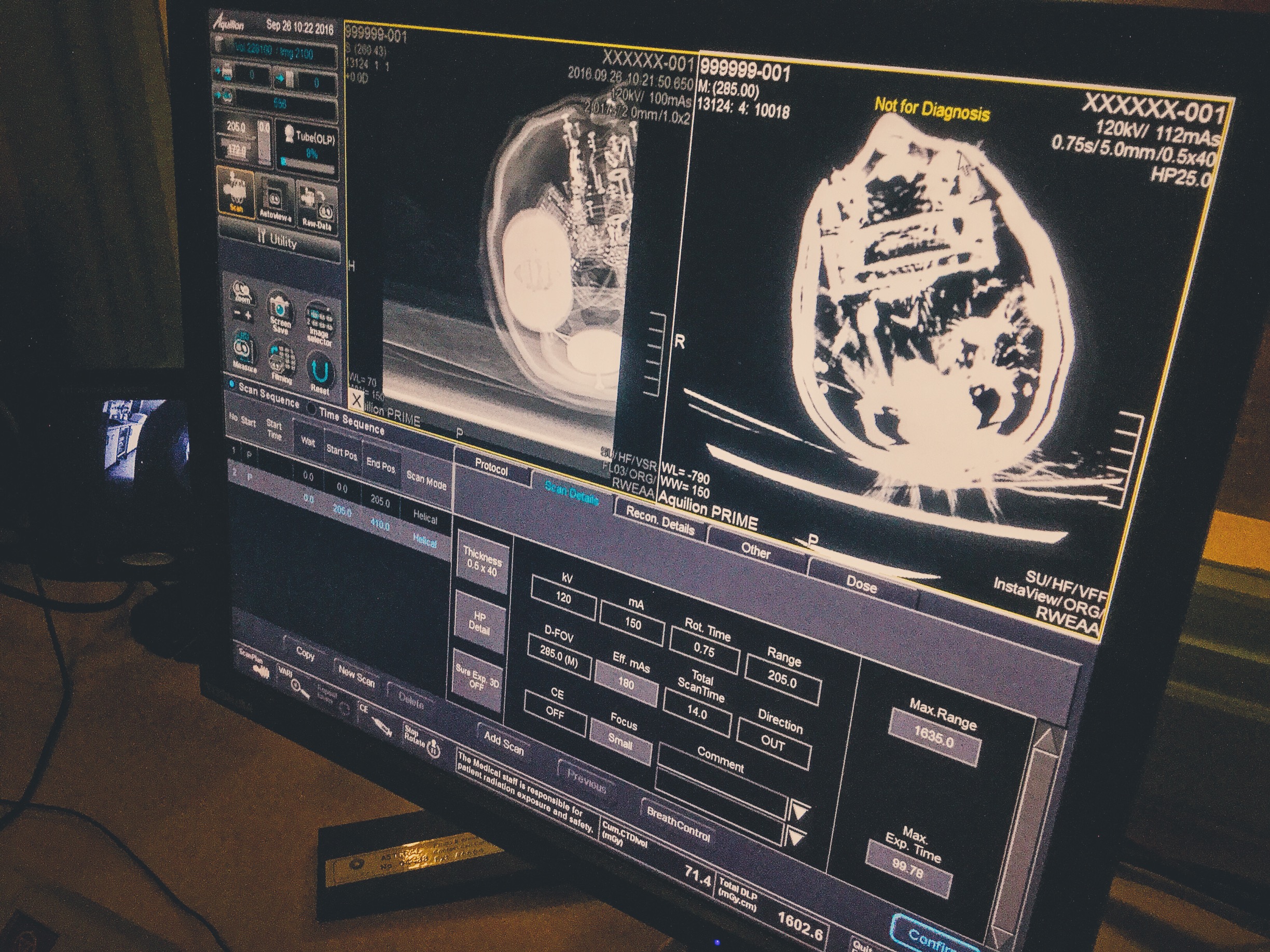
In our simulation, Tim a 5 year old boy presented via the ambulance service as a pre alert to Resus with a sudden onset headache with no history of illness or trauma. His GCS was 13 to begin with, but dropped to 8 shortly after initial assessment. Upon reassessment, he showed other signs of raised intracranial pressure including unequal pupils, raising blood pressure and falling heart rate. Following intubation and stabilisation with neuroprotective measures, he was transferred for a CT head, which revealed bilateral intraventricular haemorrhage with midline shift. Our departmental Time Critical Transfer protocol was followed and he was transferred to the neurosurgical centre. The timeline and image below shows the patient’s management within the department:
MDT Staff Feedback
This has been our largest simulation to date, involving more staff across multiple departments and services than ever before. A total of 20 staff took part in the simulation. Here is a breakdown by each team:
Paediatric ED Consultants: 1
Paediatric ED Registrars: 2
ACCS Trainee: 2
ED Nurse: 3
Children's Intensive Care Team: 3 (Consultant, SpR and Nurse)
Paediatric Anaesthetist: 1
EMAS: 2
Radiology: 2
Faculty team: 4 (including Gaumard representative)
"Excellent session which felt very real!" – Paeds ED SPR
"Brilliant training opportunity and great in sight into hospital management of these children." – EMAS crew
References:
- UHL Emergency Department: Standard Operating Procedure for Time Critical Transfer of the Sick or Injured Child
Further Reading:
- St. Emlyn's: Salt or Sugar? Hypertonic saline in raised intracranial pressure
- RCEM Learning: Decreased conscious level in a child (login required)
Learning Outcomes
The aim of Time Critical Transfer is to allow life – saving intervention which is not readily available onsite and which cannot wait for stabilisation or retrieval.
Our departmental protocol for Time Critical Transfer can be found on the hospital intranet. It gives clear instructions for contacting the paediatric anaesthetic and intensive care teams and useful checklists to facilitate safe transfer.
Once the need for Time Critical Transfer is identified, departure should occur within a maximum of 60 minutes.
Positive Feedback
SBAR handover style used to update incoming teams and short summaries given by the team leader at appropriate points to update the team and maintain situational control. This was particularly useful when there had been a clinical change and prior to important interventions or stages in patient management.
Closed loop communication demonstrated in particular during CT scan requesting and equipment preparation, initiation of neuroprotective measures and checklist completion for transfer.
Clear, honest approach taken when explaining diagnosis and management to Dad.