#SimBlog: Type 2 Respiratory Failure
“75 year old male, 2 day history of productive cough and fever. Increasing DIB and confusion.”
Observations
A – Patent
B – RR 30 Sats 97% (15L)
C – HR 120 Bp 90/70
D – GCS 14 (E4 V4 M6)
E – Temp 38°C
Clinical Findings
Bilat wheeze
Increased work of breathing
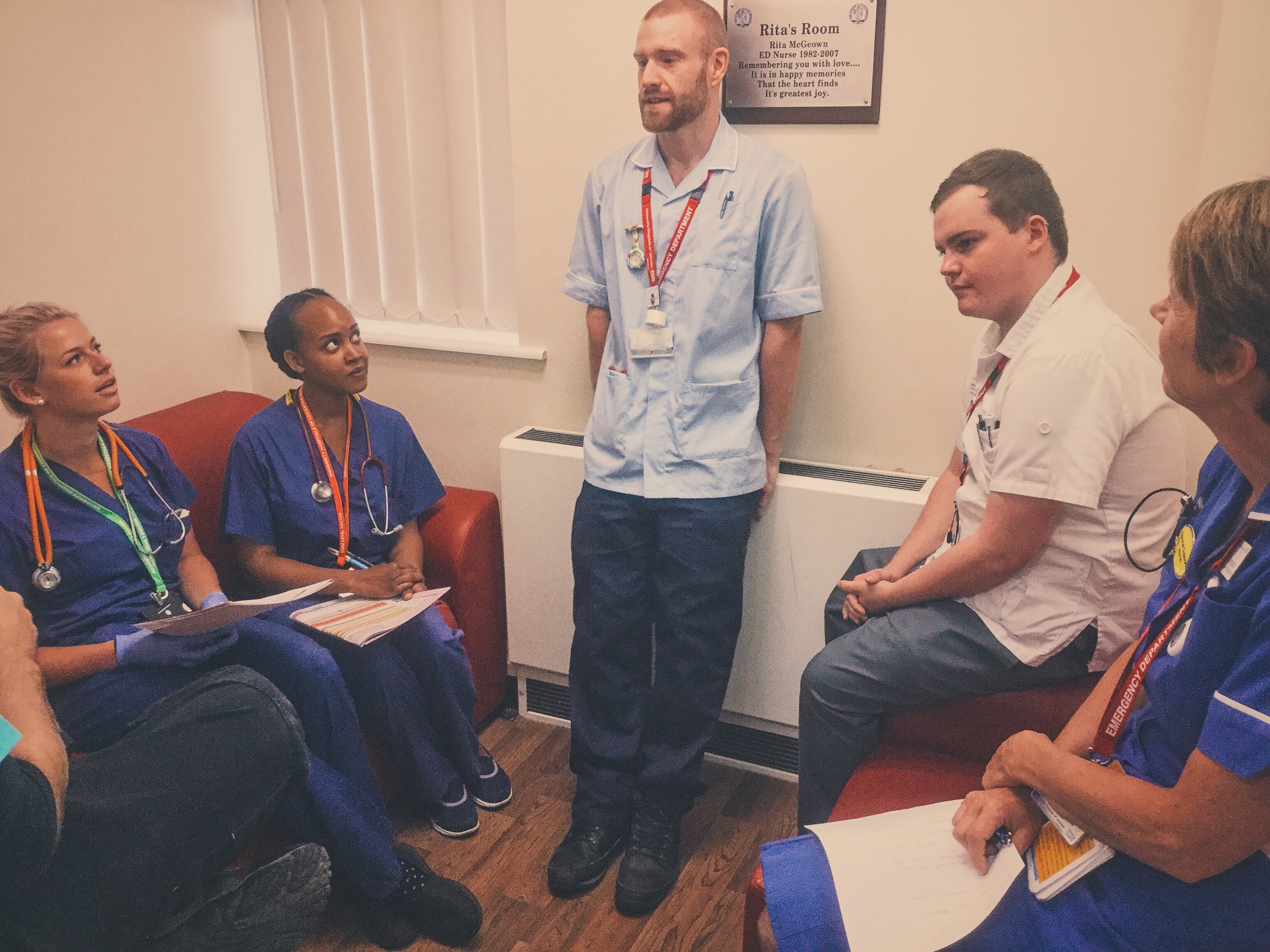
Why We Simulated
Whilst the differential for a patient who is short of breath is quite wide, many patients with a history of COPD will present in a recognisable way. It is therefore important we are familiar with the actions that are needed for this patient population and how to manage type 2 respiratory failure.
The NICE guidelines from 2010 are briefly summarised below:
Investigations:
All patients with an exacerbation of COPD should have:
CXR
ABG and the inspired oxygen concentration should be recorded
ECG (to exclude comorbidities)
FBC & urea and electrolyte concentrations
Theophylline levels in patients on theophylline therapy at admission
If sputum is purulent, a sample should be sent for microscopy and culture
Blood cultures should be taken if the patient is pyrexial
Drug Therapy:
Short acting bronchodilators: If hypercapnic or acidotic a nebuliser should be driven by compressed air, with supplemental oxygen given by nasal cannula.
Steroids: In the absence of significant contraindications oral corticosteroids should be used
Antibiotics: should be used to treat exacerbations of COPD associated with a history of more purulent sputum.
Without more purulent sputum antibiotic therapy is not needed unless there is consolidation on CXR or clinical signs of pneumonia
Intravenous theophylline: should only be used as an adjunct to the management of exacerbations of COPD if there is an inadequate response to nebulised bronchodilators.
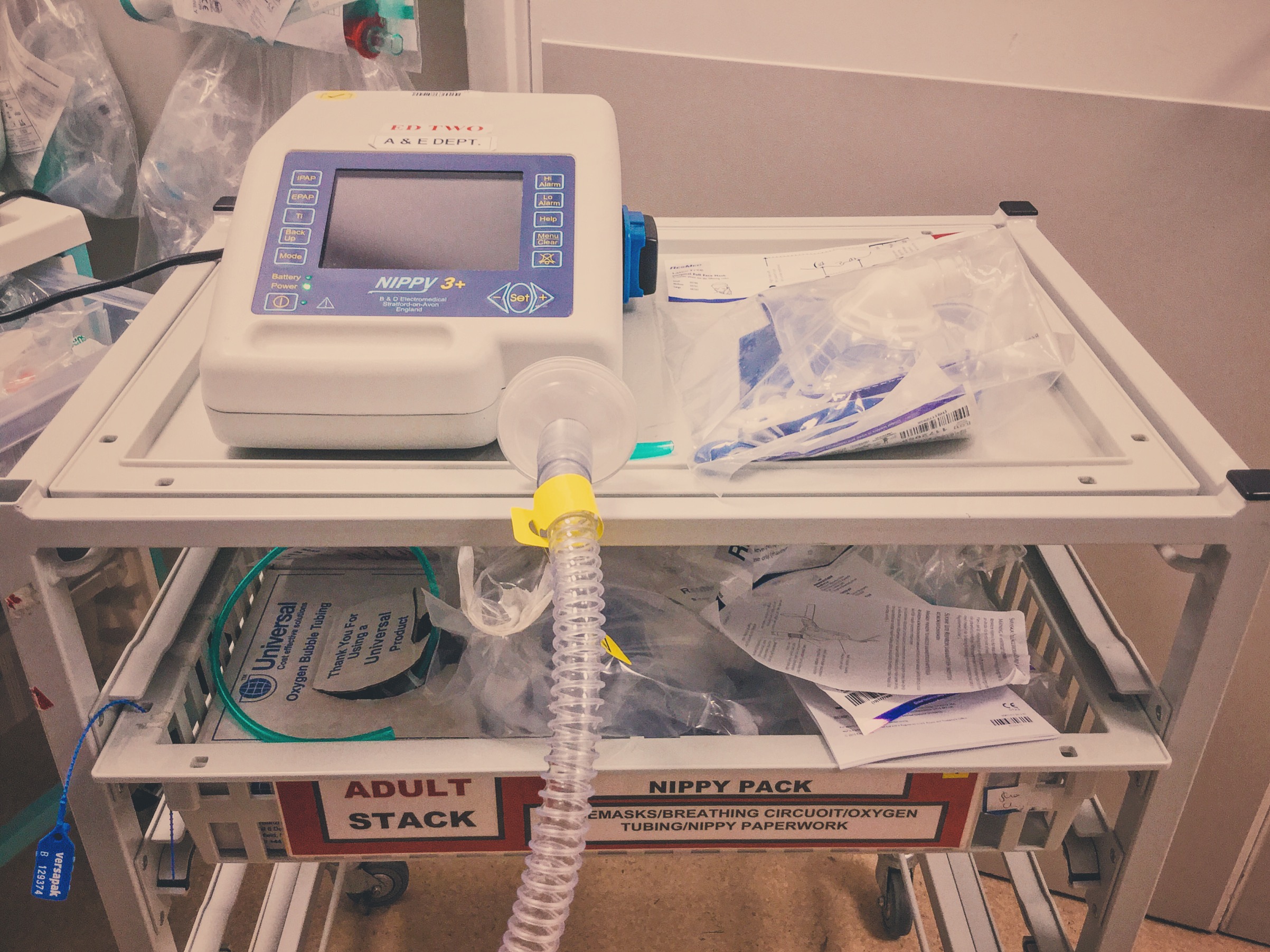
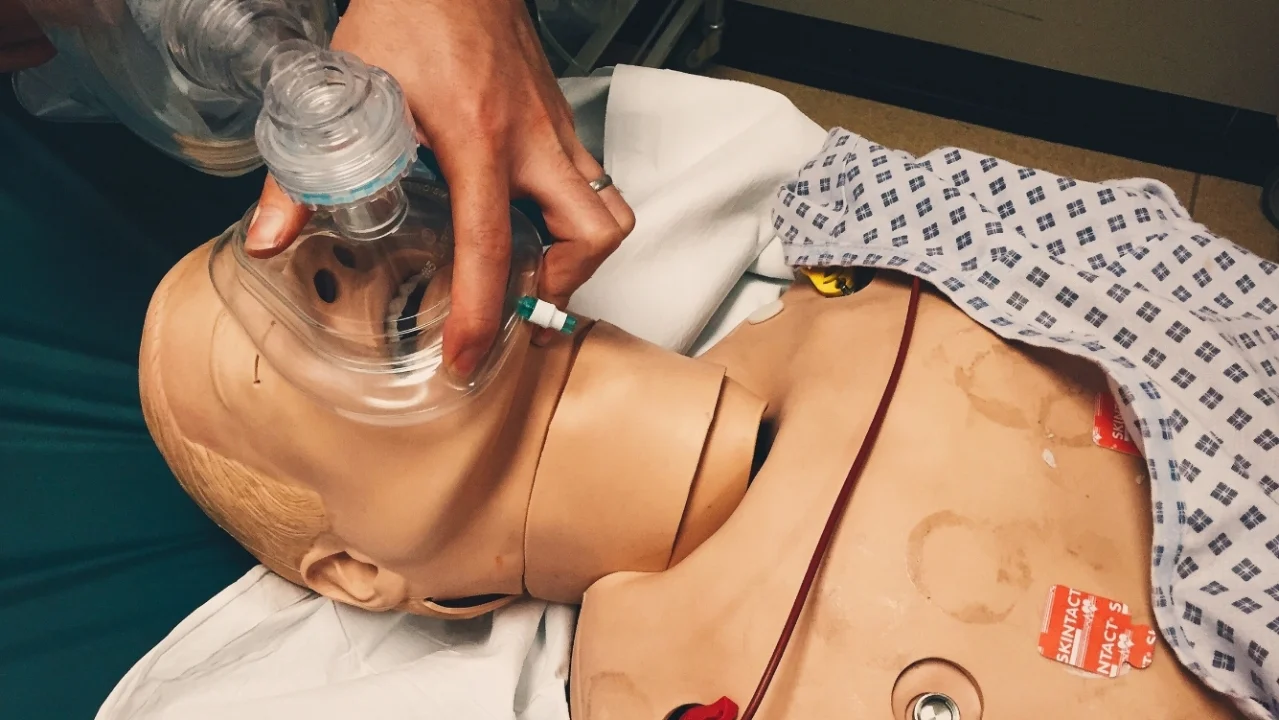
Non-Invasive Ventilation:
NIV should be used as the treatment of choice for persistent hypercapnic ventilatory failure during exacerbations despite optimal medical therapy
For patients started on NIV there should be a clear plan covering what to do in the event of deterioration & ceilings of therapy should be agreed.
Learning Points
Consider the contraindications for BiPAP/NIV – but bear in mind when this is the ceiling of treatment they may be considered as relative contraindications.
BiPAP can be uncomfortable so ensure you have warned the patient and consider holding the mask to their face to begin with rather than strapping it on.
Remember to maximise treatments as well as BiPAP, such as nebs and steroids if indicated.
Positive Feedback
Brought Team Together for discussion of findings on blood Gas.
Sought Senior Support appropriately.
Good use of the type 2 resp failure management tool.