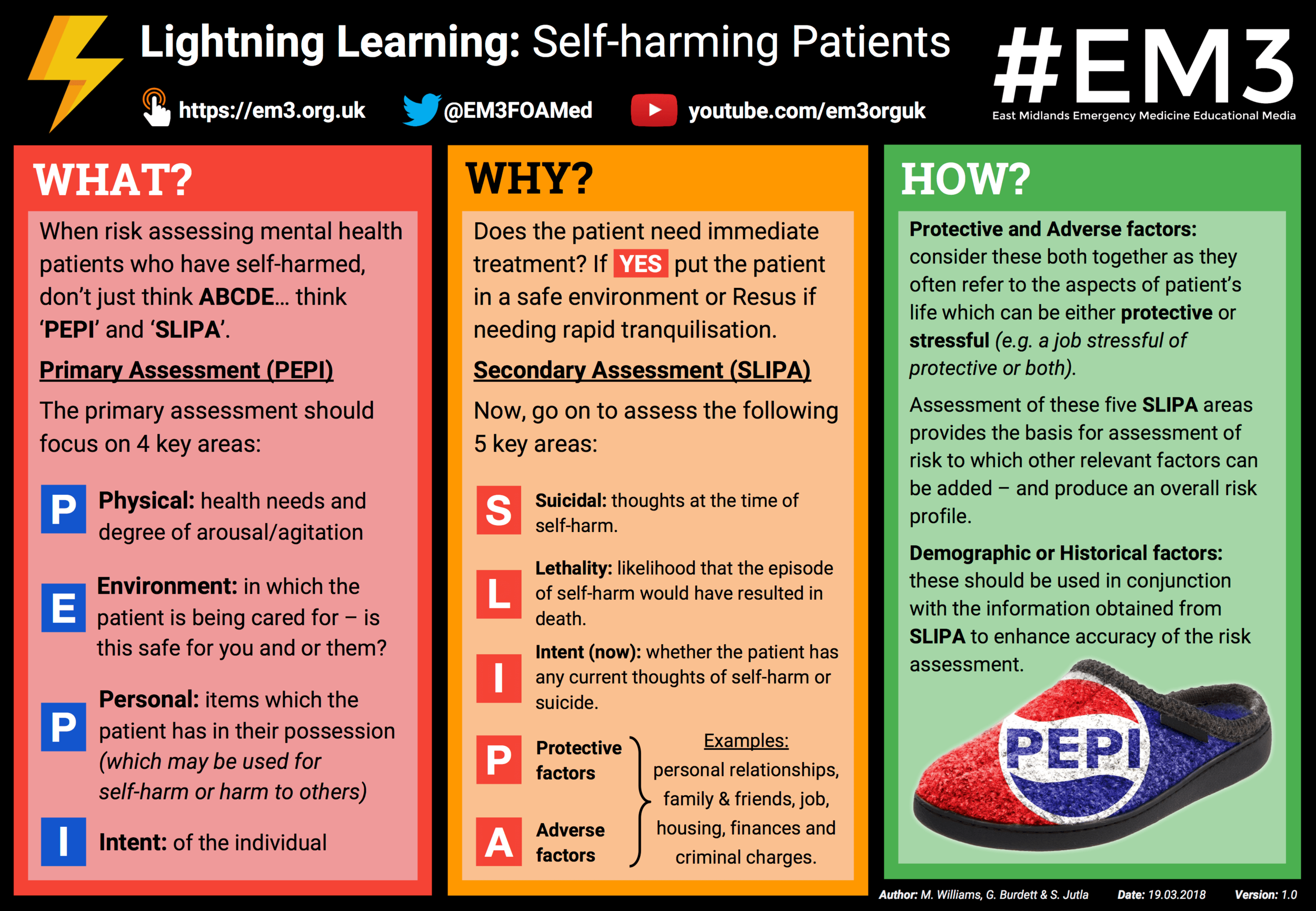
Lightning Learning: Self-Harming Patients
“When risk assessing mental health patients, don’t just think ABCDE... think PEPI and SLIPA!”
Why?
When risk assessing mental health patients who have self-harmed, don’t just think ABCDE… think ‘PEPI’ and ‘SLIPA’.
Primary Assessment (PEPI)
The primary assessment should focus on 4 key areas:
Physical: health needs and degree of arousal/agitation
Environment: in which the patient is being cared for – is this safe for you and or them?
Personal: items which the patient has in their possession (which may be used for self-harm or harm to others)
Intent: of the individual
Why?
Does the patient need immediate treatment? If YES put the patient in a safe environment (or ER) if needing rapid tranquilisation.
Secondary Assessment (SLIPA)
Now, go on to assess the following 5 key areas:
Suicidal: thoughts at the time of self-harm
Lethality: likelihood that the episode of self-harm would have resulted in death
Intent (now): whether the patient has any current thoughts of self-harm or suicide
Protective factors: e.g. personal relationships, family & friends, job, housing, finances and criminal charges
Adverse factors: same as Protective factors
How?
Protective and Adverse factors: consider these both together as they often refer to the aspects of patient’s life which can be either protective or stressful (e.g. a job stressful of protective or both).
Assessment of these five SLIPA areas provides the basis for assessment of risk to which other relevant factors can be added – and produce an overall risk profile.
Demographic or Historical factors: these should be used in conjunction with the information obtained from SLIPA to enhance accuracy of the risk assessment.