Lightning Learning: Osteomyelitis in Kids
STOP!
Osteomyelitis is an infection of the bone that causes inflammation, bony destruction, loss of limbs (and even life). Diagnosis is time-critical.
Clinical Features: Suspect in an unwell child with pain and local bony tenderness with or without pyrexia, muscle spasm or limp.
Investigations: Raised ESR, CRP and leukocytes are supportive.
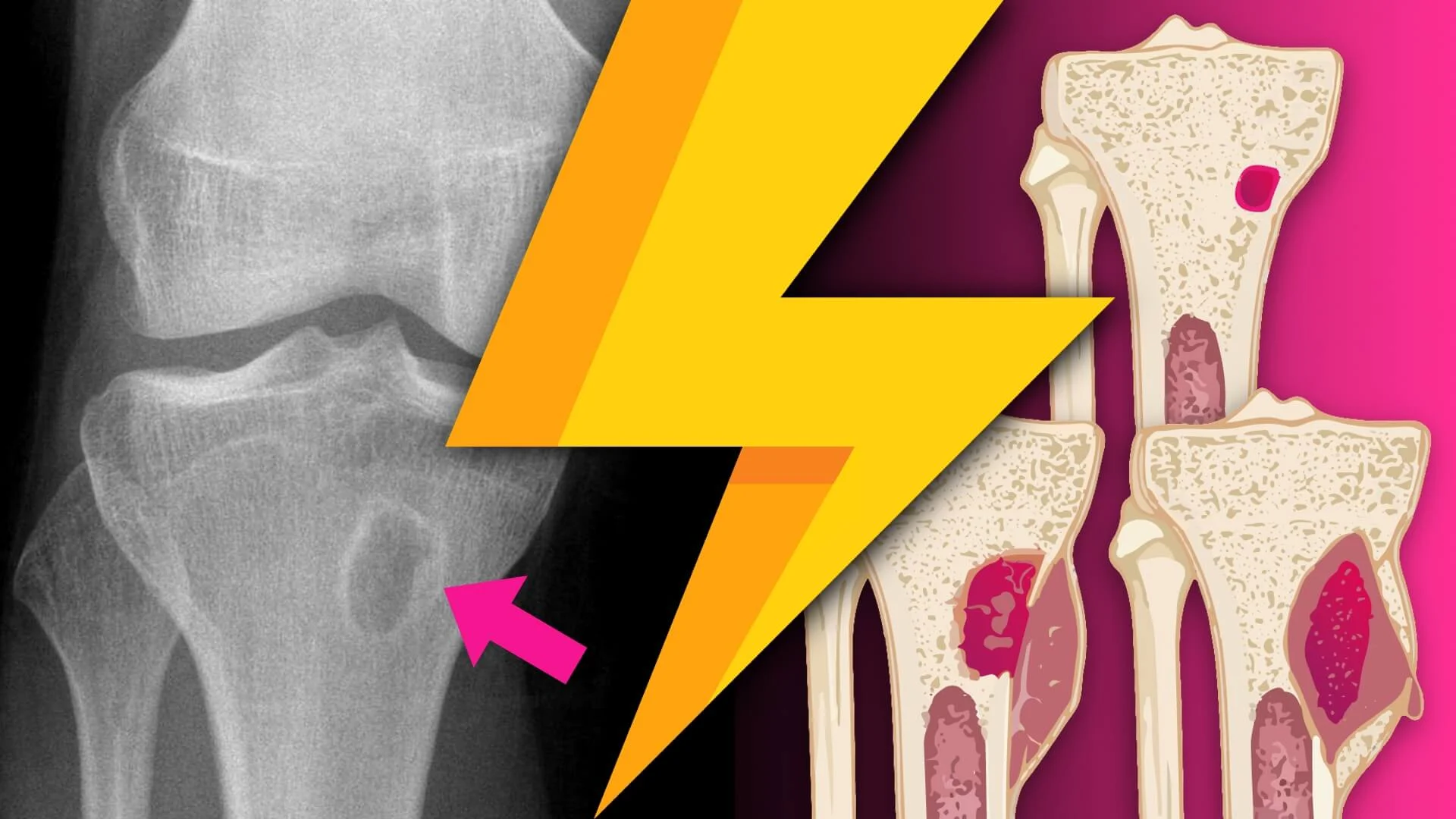
Imaging is also essential, ask…
Is there an infection?
Where is it?
Is it a drainable collection?
XR, US and MRI all have a role, though discernible findings may take 5-7 days to develop.
Blood cultures BEFORE antibiotics is an essential investigation.
LOOK
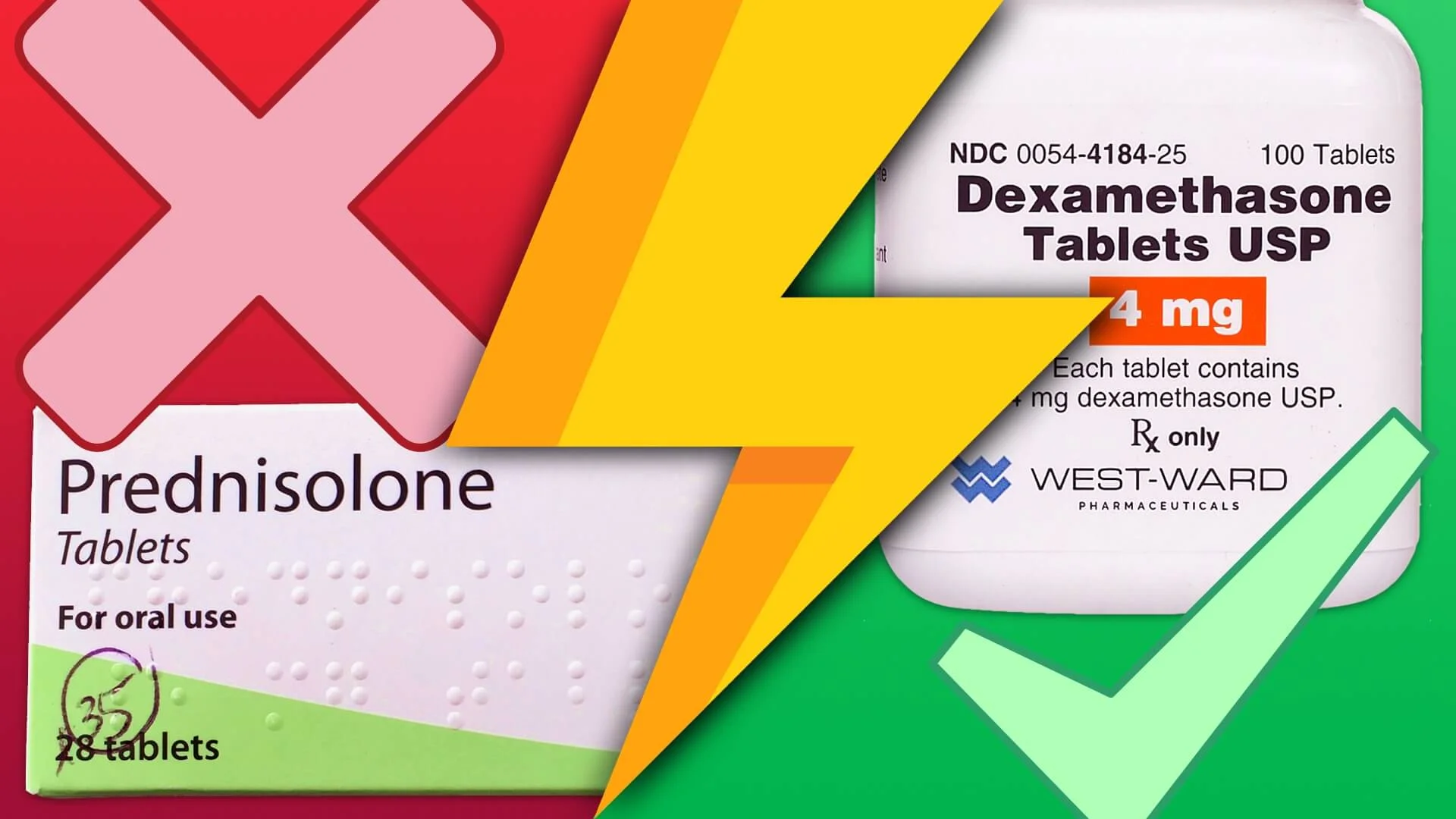
Whilst typically spread via the blood, it can also complicate cellulitis or septic arthritis and even follow on from trauma. Staphylococcus aureus is the most common bacteria implicated. Flucloxacillin is, therefore, a typical antibiotic choice.
Note: other organisms are possible depending on age (e.g. neonates → Streptococcus) and background (e.g. sickle cell → Salmonella).
Treatment: Requires prolonged IV antibiotics.
Once a diagnosis is confirmed (clinical signs, culture results, imaging) and the child is improving a switch to oral antibiotics can be considered depending on inflammatory markers, clinical state and bacterial sensitivities. Unfortunately, surgical drainage is sometimes required (~10%).
LEARN
- Hematogenous Osteomyelitis in Infants and Children: Imaging of a Changing Disease (D. Jaramillo et al.)
- Osteomyelitis in Kids (Ped EM Morsels)
- Haematogenous osteomyelitis in children: epidemiology, classification, aetiology and treatment (A. Baker et al.)