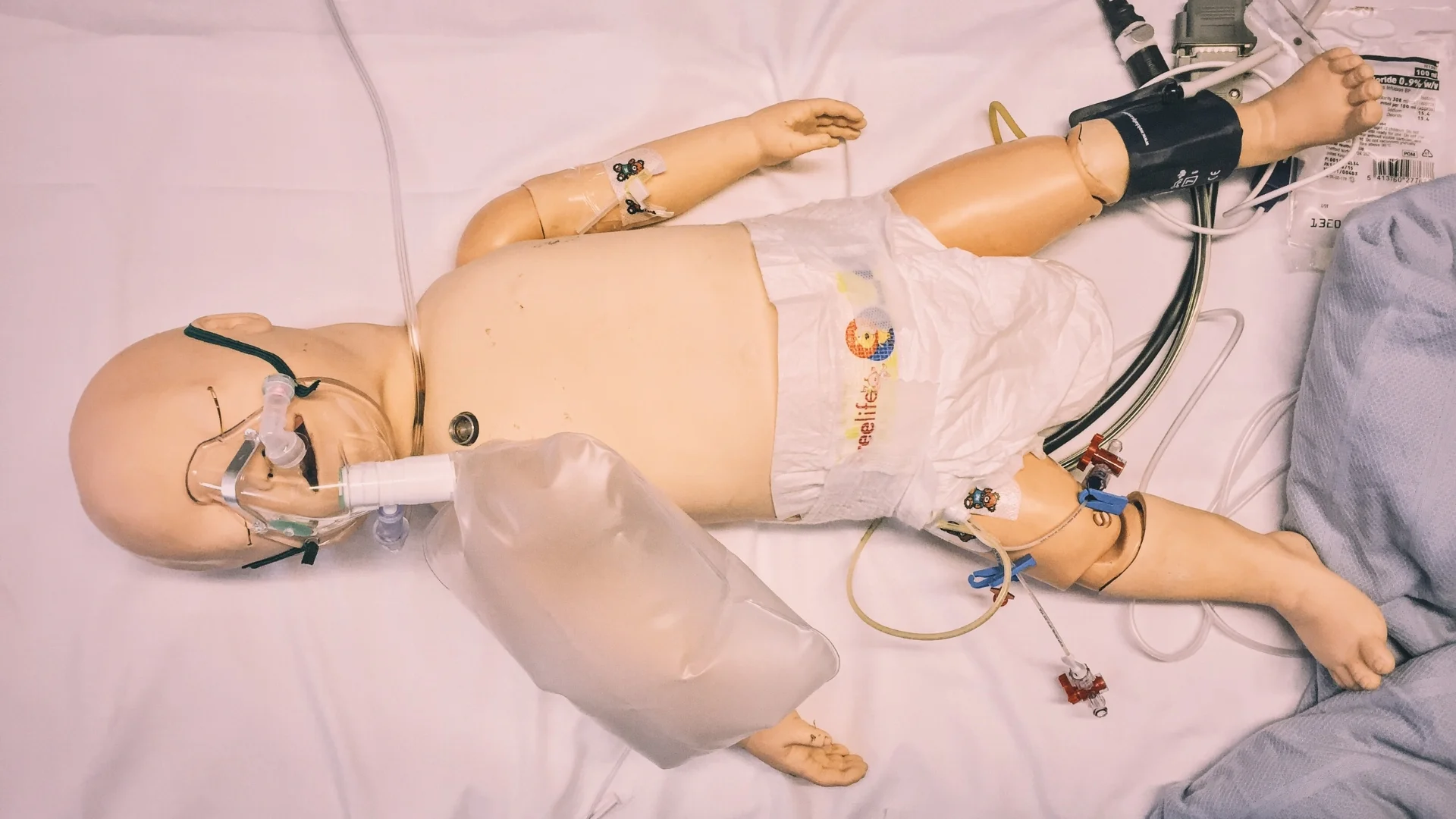
#SimBlog: Cardiac Baby
““A 5-day-old baby girl is brought to ED by mum with poor feeding, sleepiness and fast breathing.””
Observations
A – Patent
B – RR 60, sats 90%
C – HR 170, BP 45/30, CRT 4 seconds
D – Quiet but responsive
E – Temp 37°C
Clinical findings
Tachypnoeic but clear chest with no recessions
Systolic murmur
Absent femoral pulses
Why we simulated?
Congenital heart disease is one of the most common types of birth defect, affecting up to 9 in every 1,000 babies born in the UK. Although many of those affected are now identified by antenatal scanning or during the newborn baby check, some first present to the ED within a few days of life. This is because at this time the heart is still undergoing changes, converting from the foetal to neonatal circulation.
One of the major structural changes is the closure of the ductus arteriosus, a connection between the pulmonary artery and the descending aorta. This reveals those who are dependent upon this duct to enable mixing of blood to maintain their systemic or pulmonary circulations.
Presentation of duct dependent lesions can vary widely from subtle symptoms of poor feeding, sleepiness and slightly fast breathing when the duct is starting to close, to the collapsed baby in cardiogenic shock where closure is imminent. This can often be a diagnostic challenge, since the decompensated patient with sepsis or an inborn error or metabolism can have a very similar presentation.
It is therefore important that the team working in ED can recognise the signs of duct dependent cardiac disease and follow the appropriate management steps to ensure the patient is stabilised and transferred to the appropriate speciality.
Please find attached the University Hospitals of Leicester Guidelines for Dinoprostone infusion and Management of the Critically Unwell Child.
Further Reading:
- Children's Heart Institute homepage
- Just another bronchiolitis? – Don't Forget The Bubbles
Learning outcomes
If the patient has not responded to treatment in the way you expect then reconsider your differential diagnoses.
Verbalise your thoughts and share them openly and clearly with the team.
Be specific with what you are asking for when contacting other specialities – you are much more likely to get the help you need!
Positive feedback
Systematic ABC approach.
Allocated roles appropriately within the team.
Sought advice and review from seniors and appropriate specialities when the patient’s condition failed to improve with initial management steps.