#SimBlog: Alcohol Withdrawal
“A 46-year-old man who has been admitted to EDU on an alcohol pathway. He has been on the ward for a few hours to sober up. He usually drinks throughout the day and is due to be discharged later.”
Observations
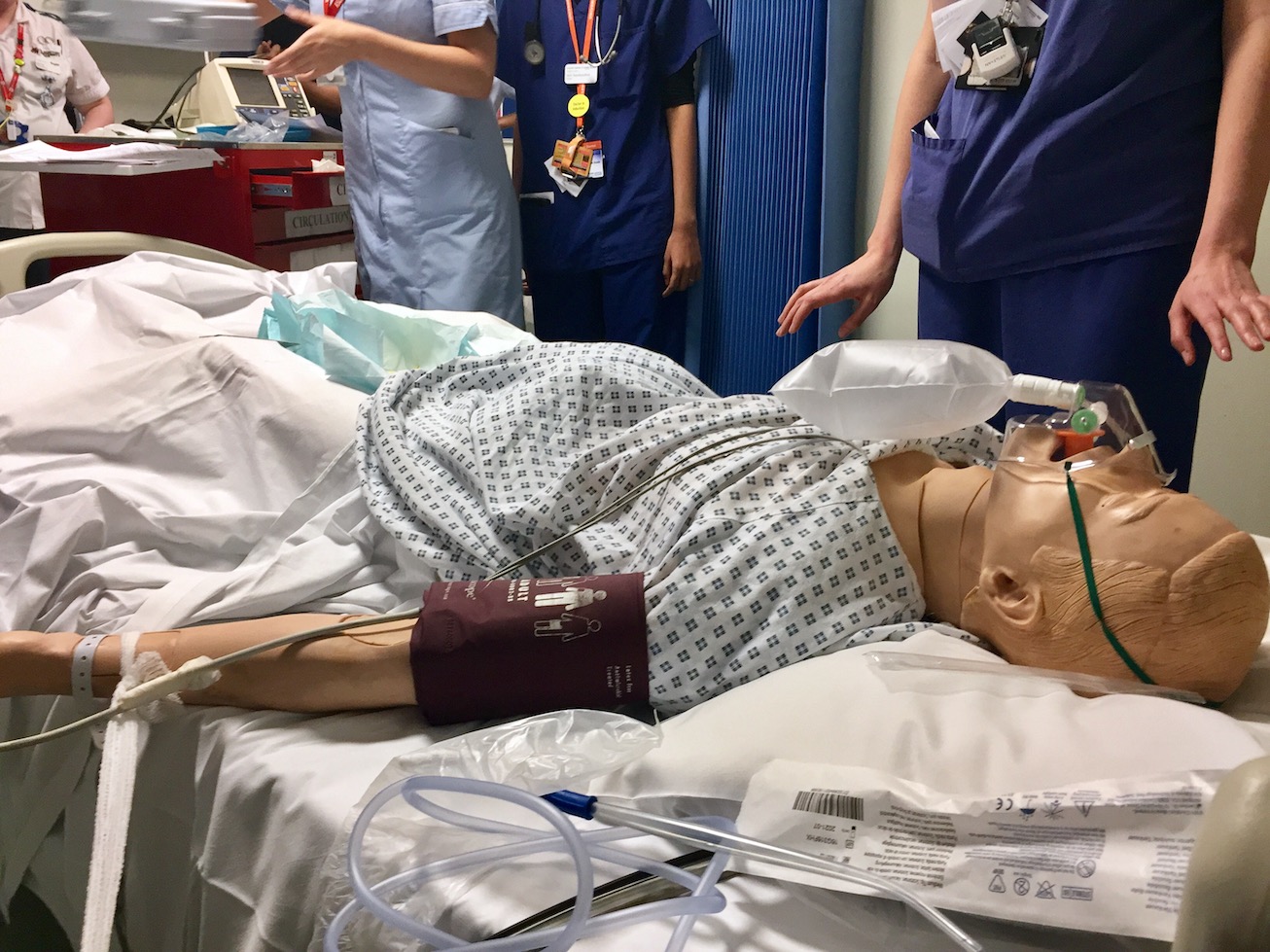
A – Obstructed airway which is full of secretions
B – RR18, sats 83% on air
C – HR 120, BP 140/75
D – Actively seizing
E – 37.2°C
Clinical Findings
Actively seizing
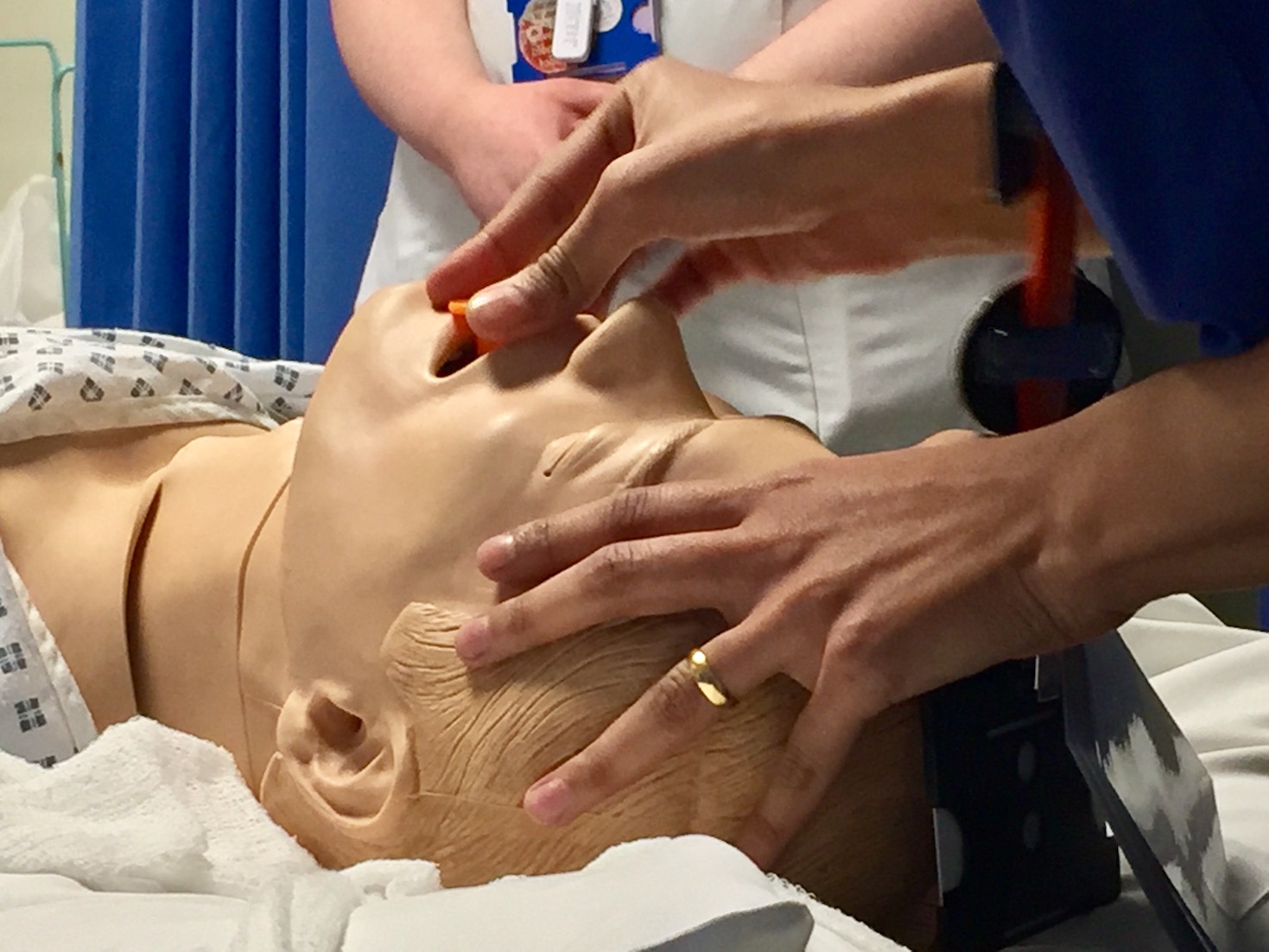
Airway required suctioning and insertion of OPA
BM 9
Equal pupils
Low saturations
Why Did We Sim?
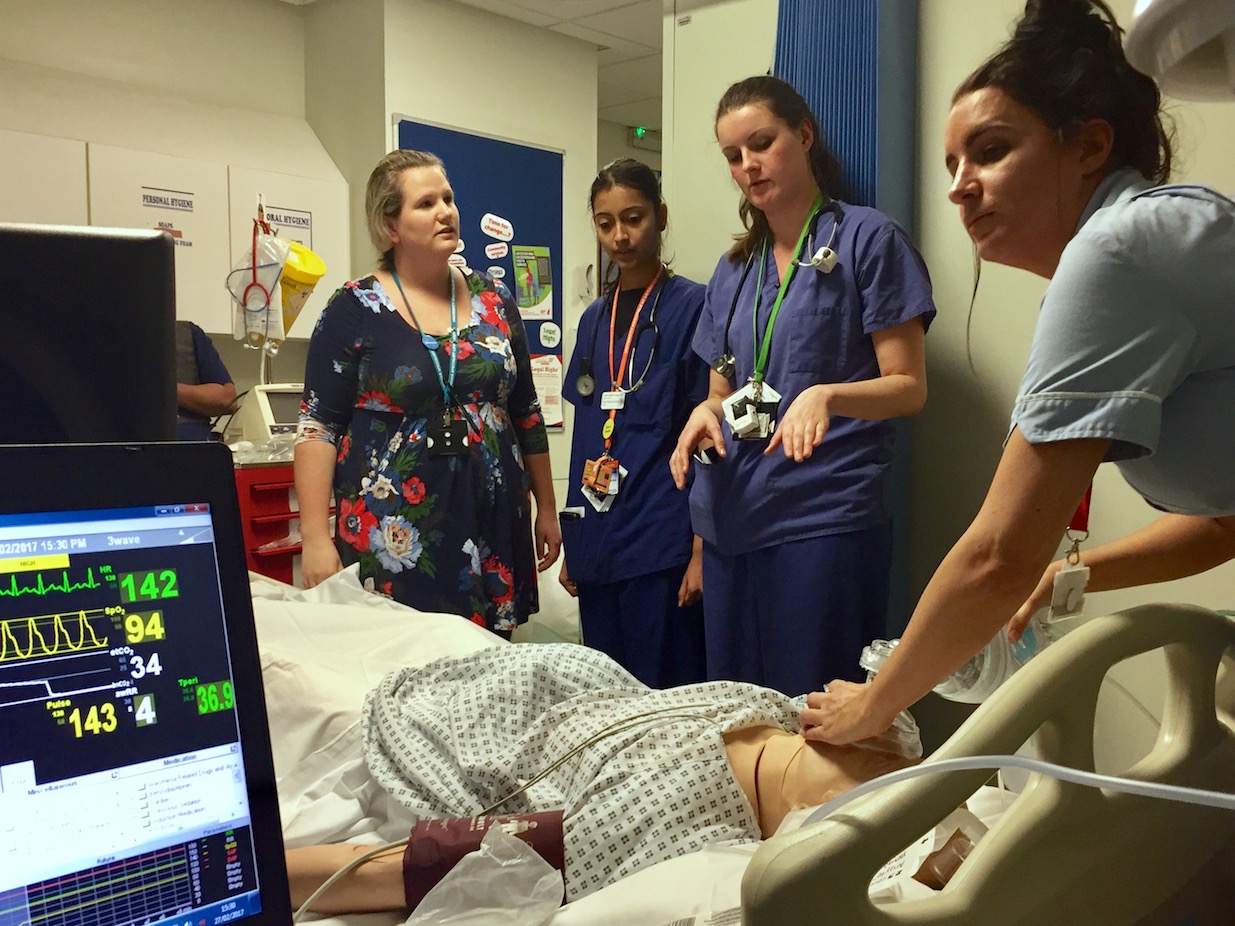
Patients are often admitted to our Emergency Decisions Unit (EDU) on alcohol pathways to monitor them as the effects of intoxication wear off. Our EDU staff are often relatively junior, so it is imperative they know how to manage complications.
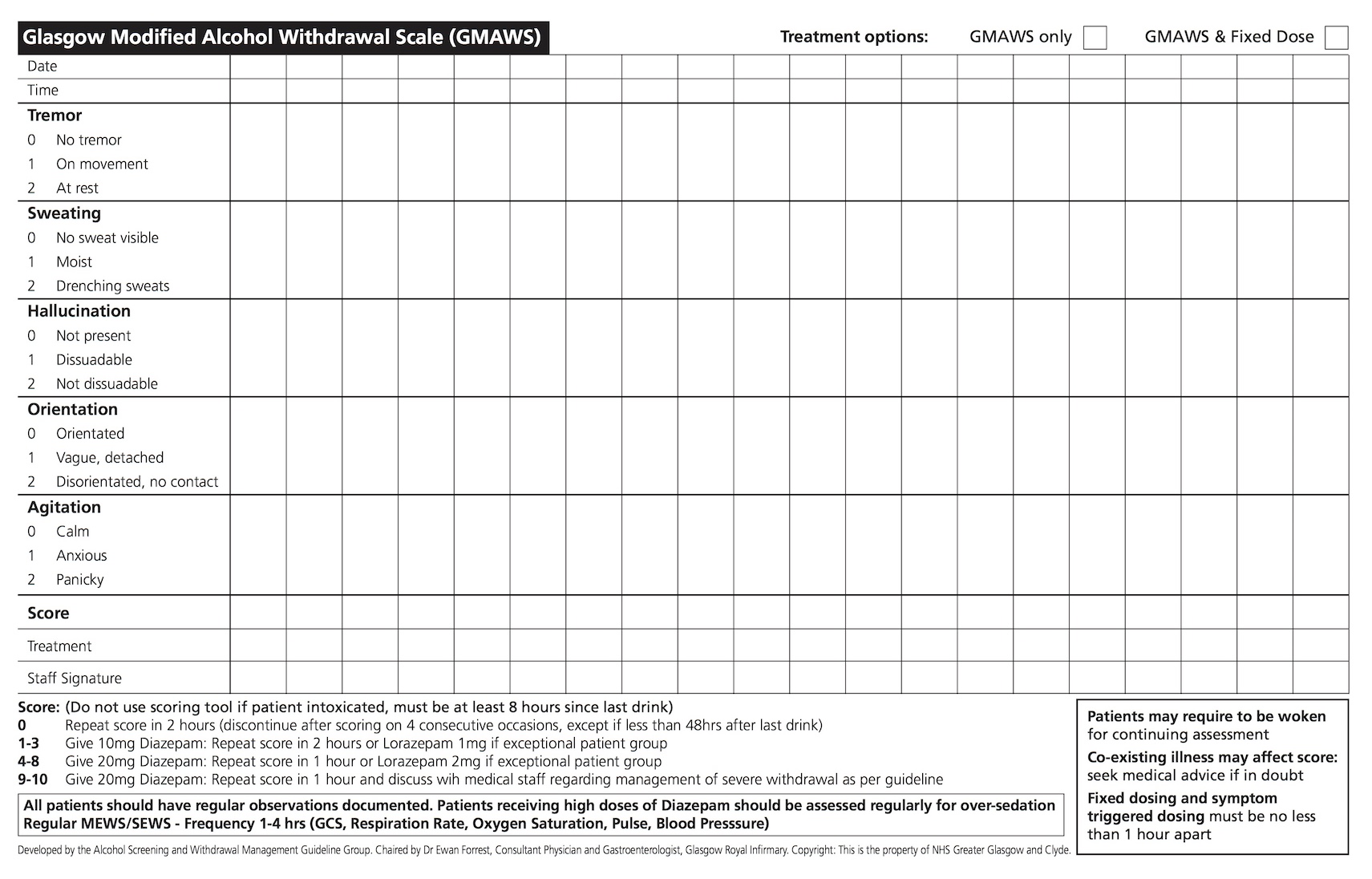
Patients are at higher risk of fitting if they go long periods without alcohol, but this can be after as little as two hours. Alcohol withdrawal presents with a spectrum of symptoms including tremor, sweating, hallucinations, orientation and agitation.
These symptoms should be monitored on a regular basis and treatment provided to halt the progression of these features. If treatment with benzodiazepines is not given, symptoms can progress, and the patient could have seizures and develop delirium tremens (which is a medical emergency).
Locally we use the Glasgow Modified Alcohol Withdrawal Scale (GMAWS), which allows us to monitor the patient’s symptoms. The scale advises a dose of diazepam based on which symptoms are present, and their severity. If a patient does have a withdrawal seizure (which is not self-terminating) it is treated with benzodiazepines. Lorazepam 4mg can be given twice, although it is advisable to titrate to effect. Benzodiazepines are a respiratory depressant, so if too much is administered, it can cause a low respiratory rate or respiratory arrest.
It is worth noting that patients will react differently to these drugs, and it is possible to cause such complications with the advised therapeutic dose. Always be prepared and know what to do if a respiratory arrest does occur. As long as you are able to maintain an airway and can ventilate the patient, the lorazepam should wear off and the patient will start breathing for themselves. If they do not you will need to involve ITU and avoid flumazenil, as it will inhibit benzodiazepine receptors. So if the patient fits again – it will be difficult to stop.
Further Reading:
- NICE Guidance: Alcohol-use disorders: diagnosis and management of physical complications
- University Hospitals of Leicester (UHL) policy: Acute Alcohol Withdrawal Management
Learning Outcomes
Titrate dose of lorazepam to effect.
If respiratory rate drops, ventilate the patient via BVM – avoid flumazenil.
If trismus occurs, insert NPA.
Positive Feedback
Good ABC approach.
Good use of re-assessment and summaries.
Team leader acknowledged limitations and called for help while ensuring the patient was safe.