#SimBlog: Sepsis Mimics
WARNING: this post pre-dates SEPSIS 3.0 & may refer to older definitions
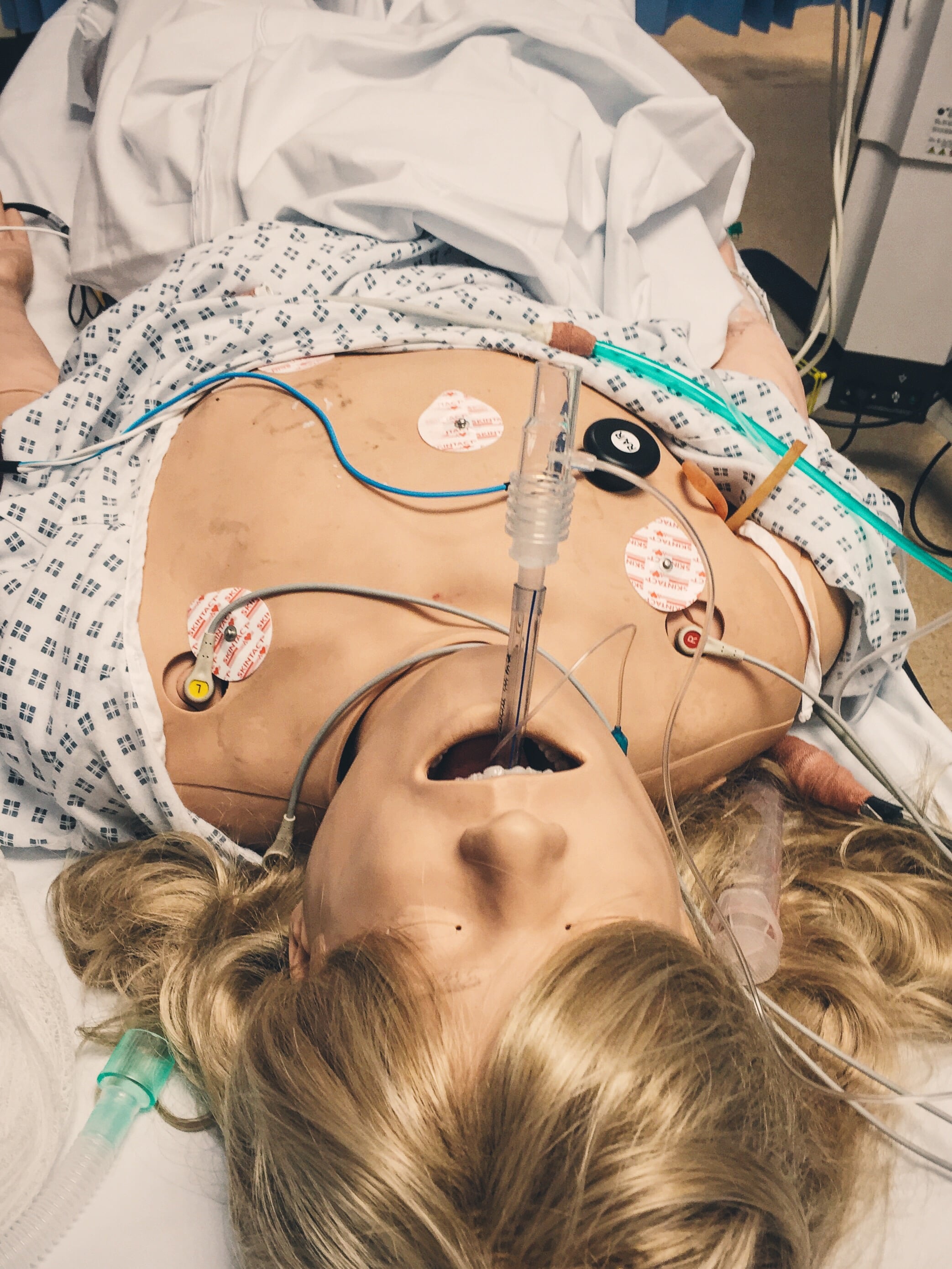
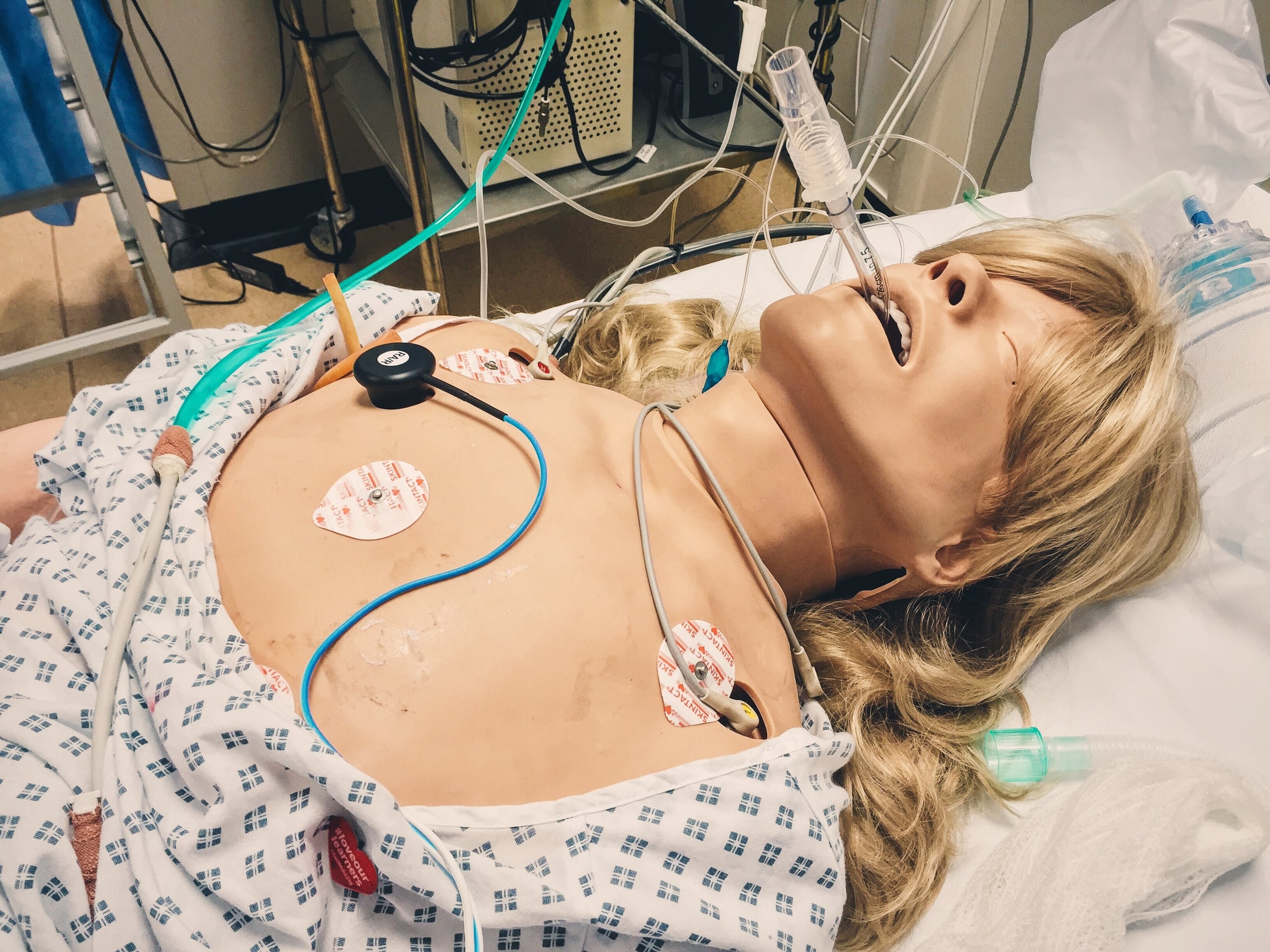
““21-year-old female brought in by ambulance. Acute onset DIB, tachycardic & tachypnoeic, pre-alerted as ?sepsis””
Observations
A – Clear & self-maintaining
B – RR 32, SpO2 92%
C – HR 127, BP 79/60
D – GCS 15/15, PERL
E – Temp 37.8
Clinical Findings
Clammy & cool peripheries
Normal percussion note on chest examination
Auscultation of chest reveals good bilateral air entry
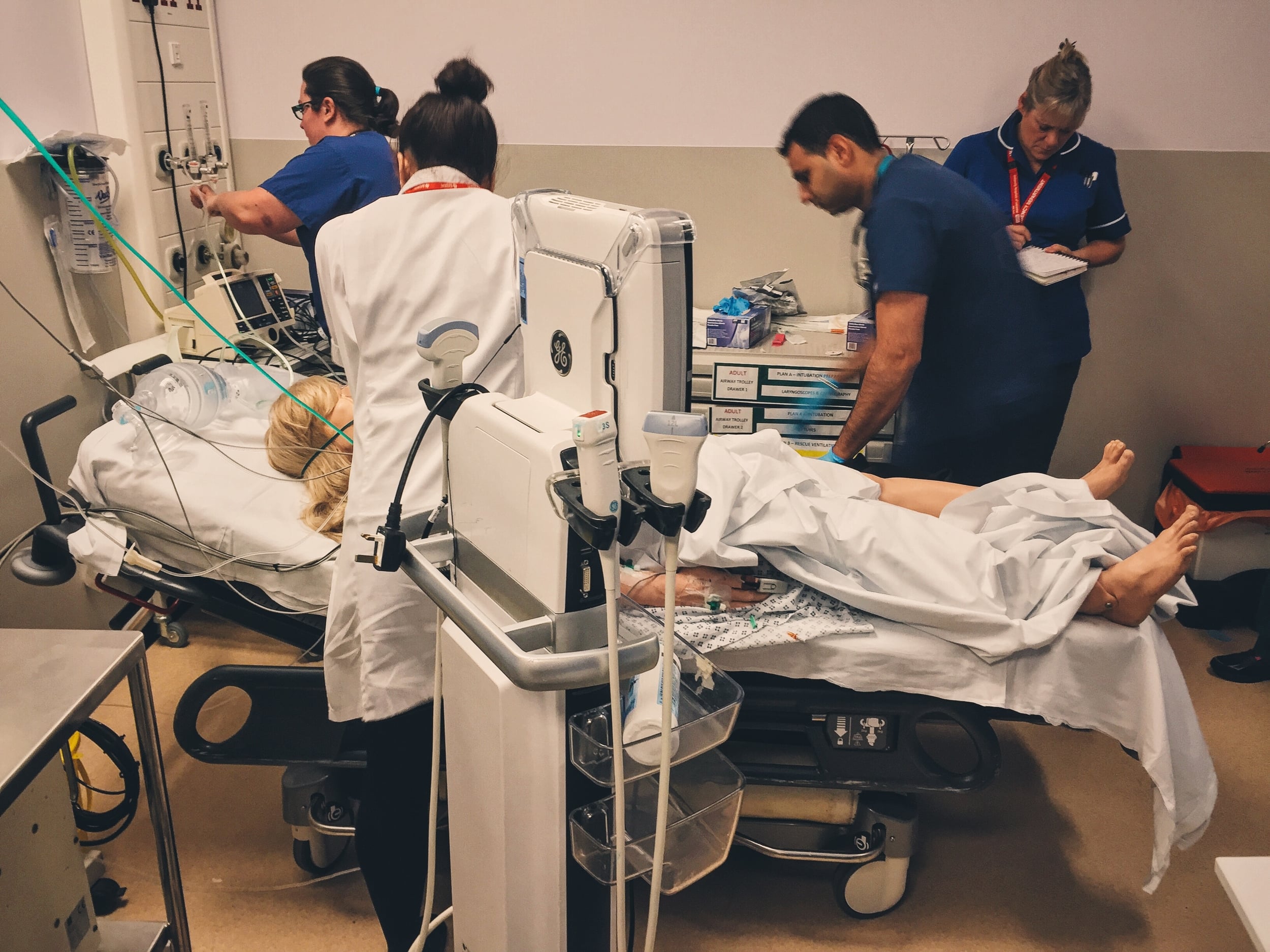
Why We Simulated
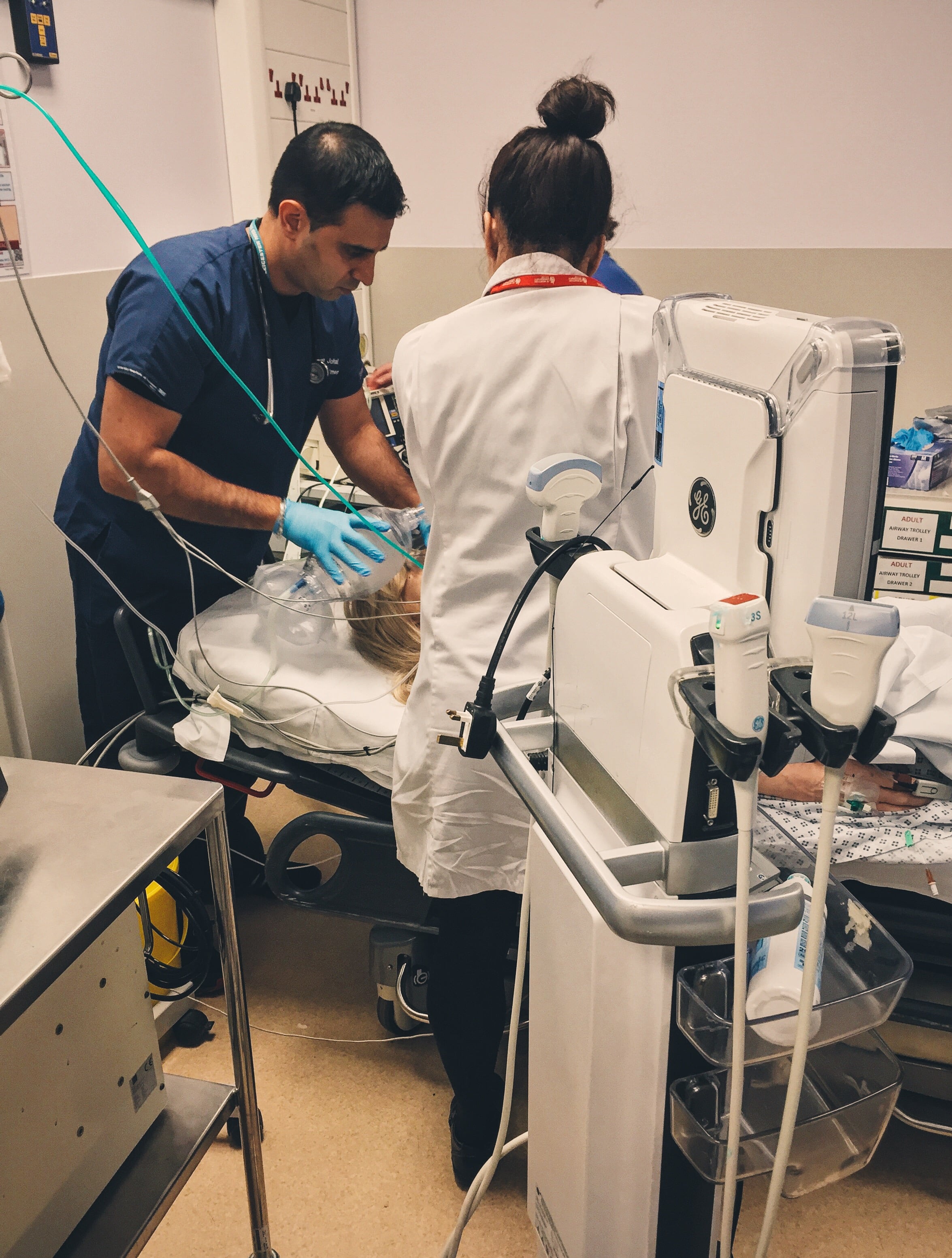
Patients presenting to the ED with evidence of shock or SIRS positive are identified as unwell – however it is not always easy to identify the underlying cause.
A lot of work has gone into identifying patients with Sepsis as the mortality for Severe Sepsis (also known as RED FLAG SEPSIS) is high. As emergency physicians we need to be able to identify and treat these patients appropriately. However we also need to be aware of the SEPSIS MIMICs as failure to identify these can lead to misdiagnosis and incorrect treatment.
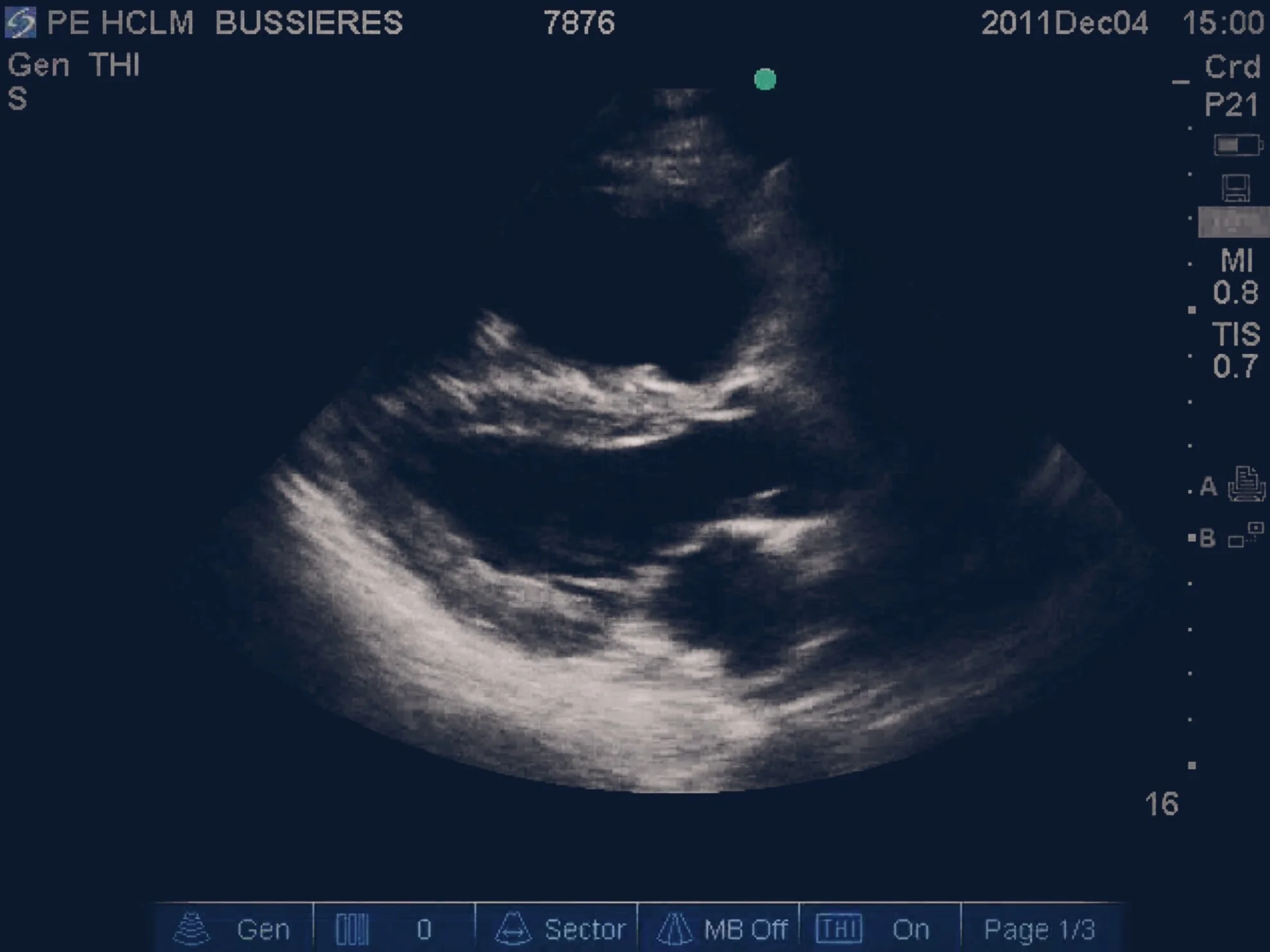
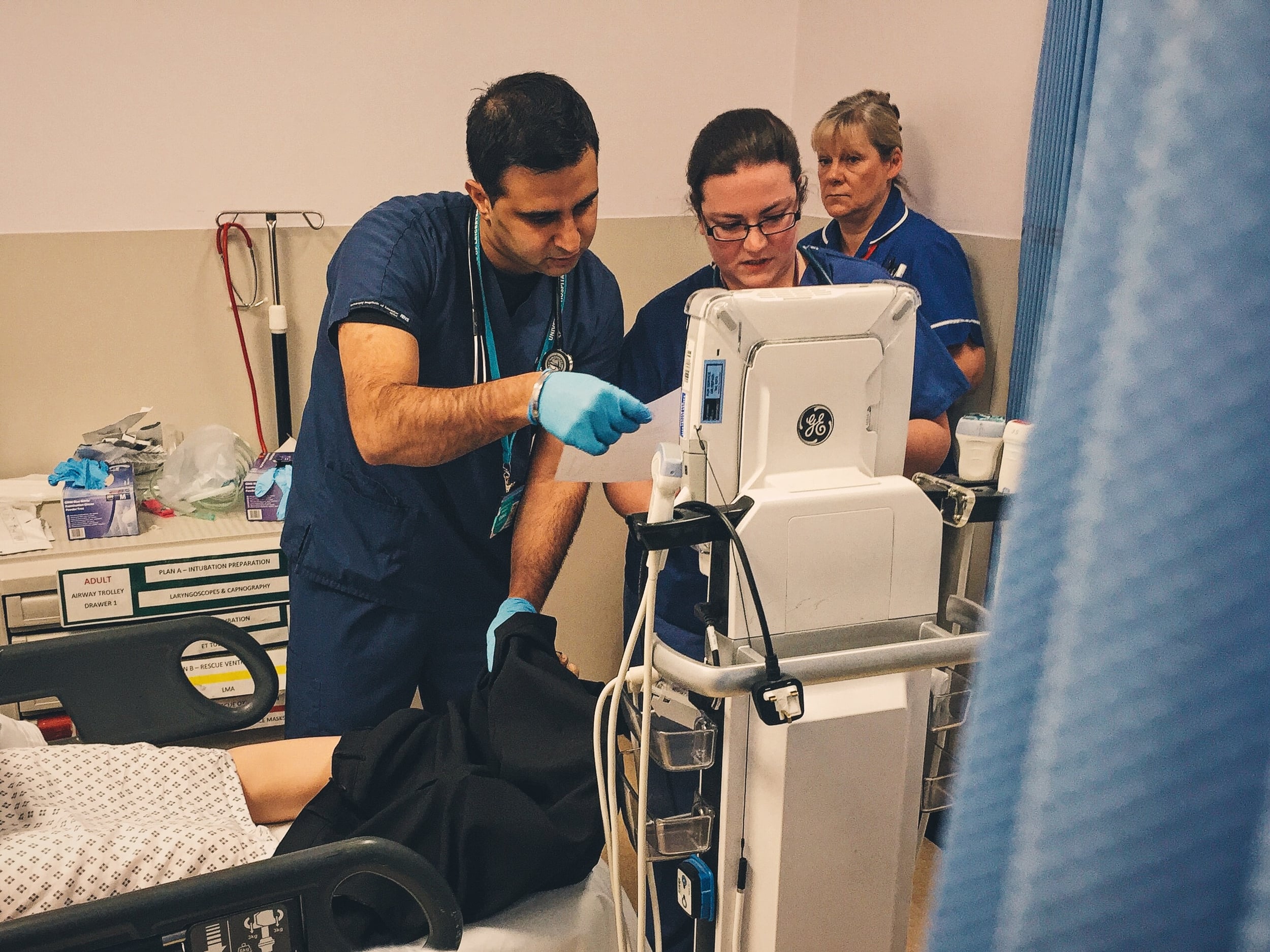
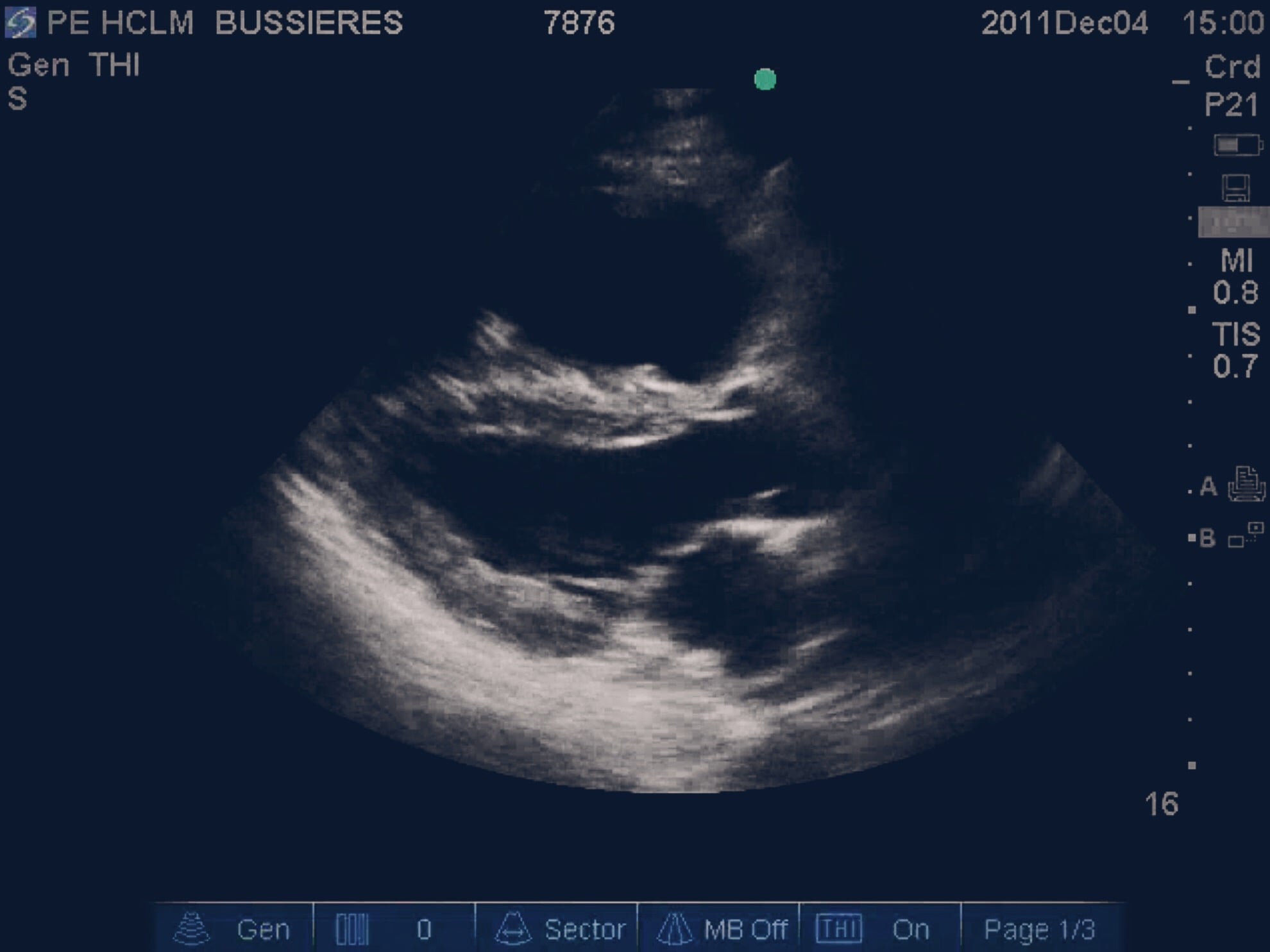
Pulmonary Embolism is one such diagnosis as it can cause a patient to present with SIRS and can cause a patient to present with shock. Diagnosis requires clinical suspicion and may well need imaging to confirm it (bedside Echo may be helpful). Treatment for a shocked patient or a patient in cardiac arrest should include considering thrombolysis with Alteplase.
As a final pearl if you see a patient or a junior discusses a patient with SEPSIS but you cannot find a clear source – stop and think are you missing a MIMIC.
Further Reading:
- EMDOCs – Sepsis Mimics
- NICE – VTE Guideline
- #EM3: Lightning Learning – VTE
- Life in the Fast Lane – Thrombolysis in submassive PE
Learning Outcomes
We have a trust policy for Thrombolysis in PE.
Within our trust we use Alteplase as our thrombolytic agent.
When asking for something be specific about who you ask – try to avoid asking "someone".
Positive Feedback
Good consideration of Sepsis Mimics in a SIRS positive patient.
Team leader shared mental model to ensure all team members were aware of next steps in management.
Team well briefed and prepared prior to patient arrival.