Elevated Troponin: Always A Cardiac Problem?
Stroke & Subarachnoid Haemorrhage
Patients with intracranial bleeding and catecholamine release, either in plasma concentration or stimulated specifically in cardiac nerves, can cause “contraction band necrosis” in the myocardium. This necrosis of cardiac cells releases troponin. It has also been suggested that the higher level of troponin elevation in subarachnoid haemorrhage suggests a higher severity of injury and a poorer prognosis. However, in patients with ischaemic strokes, there are not as strong of studies to correlate with prognosis.
Embolism, Hypertension & Acute Pulmonary Oedema
An increase in troponin correlates an increased morbidity and mortality in patients with acute PE. Do not assume a patient with a positive troponin result will have had an NSTEMI without first considering the diagnosis of PE. Consider patient risk factors and patient history and examination. If suspicious of PE, use a clinical scoring system (wells score) to prioritise the patient and consider confirmatory tests. Troponin elevation in this setting of PE signifies a worsening clinical picture. The patients with a PE and elevated troponin are likely to deteriorate and will warrant early admission for close monitoring and treatment.
Chronic Obstructive Pulmonary Disease (COPD)
Myocardial damage occurs during a COPD exacerbation secondary to increased left ventricular afterload, increased demand, pulmonary hypertension, hypercapnia, and hypoxia that puts more demands on energy needs from the body. Elevated troponin in this setting has actually been proven to be a strong independent predictor of mortality in those admitted, later treated and discharged. It is also a predictor of increased need for non-invasive mechanical ventilation. Unfortunately, these patients often have other comorbidities that predispose them to acute coronary syndrome.
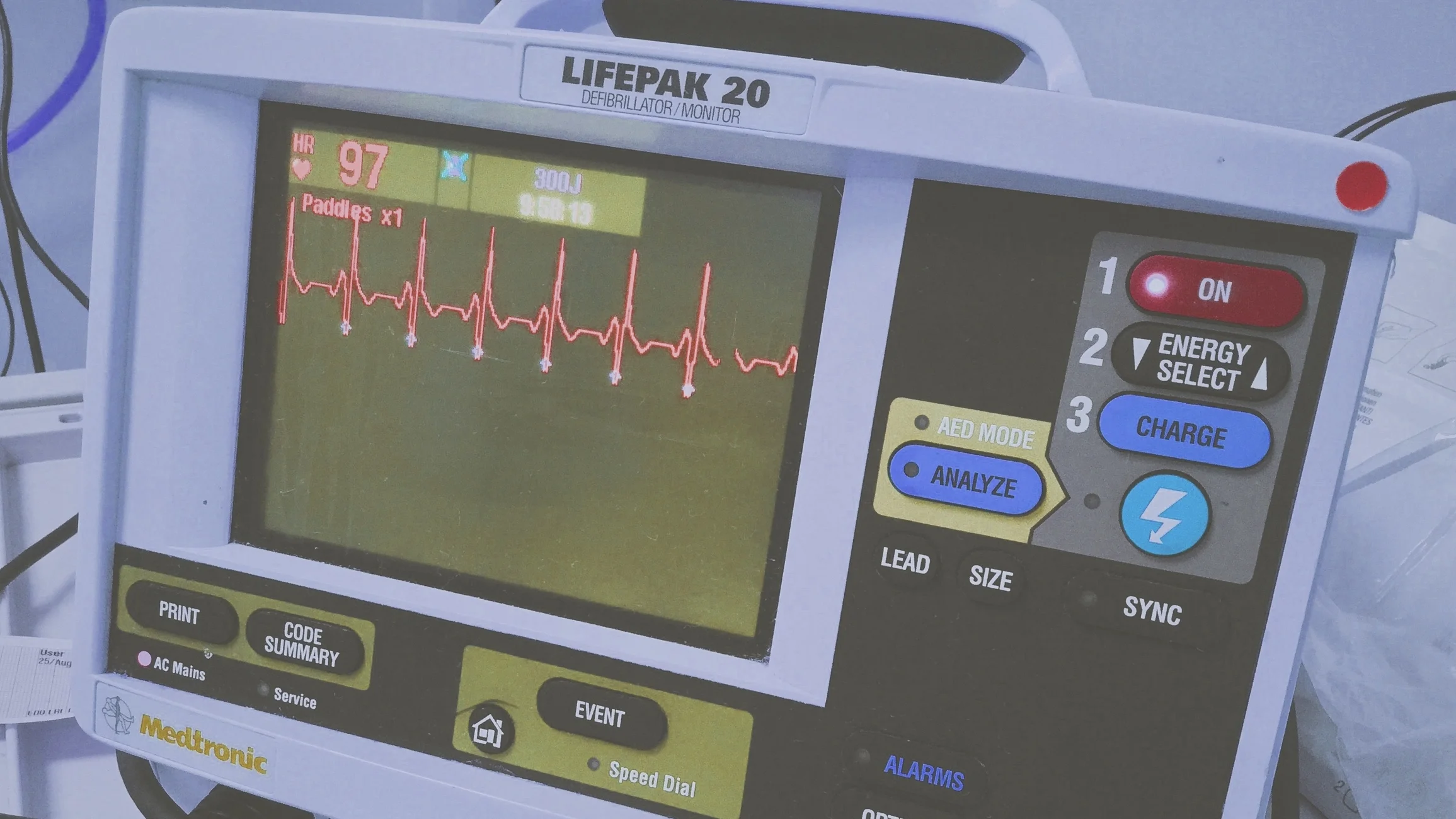
Acute Coronary Syndrome (ACS)
ACS constitute a large spectrum of clinical conditions ranging from unstable angina pectoris to acute ST-elevation myocardial infarction (STEMI). Chest pain is usually the major symptom of atherosclerotic heart disease; however, it may be challenging to diagnose correctly, especially in the emergency department, due to the ambiguous way individuals characterise pain. Cardiac serum markers, especially cardiac troponins are the cornerstone of the diagnosis, risk assessment and treatment. To diagnose acute coronary syndrome, you need two out of three of the following: clinical features, new or dynamic ECG changes of ischaemia, troponin elevation. An interventional management strategy (angiography/stenting) is beneficial for plaque rupture coronary events which have caused genuine acute coronary syndrome.
Chronic Kidney Disease (CKD)
There are many possibilities as to why the troponin is elevated in this patient population including decreased clearance of normal cardiac myocyte loss, heart failure without evidence of ischemia or infarct, chronic inflammation or damage to skeletal muscle, or a combination of them all. So how are we supposed to approach this clinically? Practitioners should consider the entire picture of the patient from their presenting symptoms to their ECG and lab results with comparison to prior results (if available). It is thought that cardiac troponin (I) holds advantages over troponin (T) because it is cleared more by dialysis and undergoes more chemical conversions in serum due to its instability. Troponin (I) should be less elevated than troponin T in the setting of chronic renal failure. The clinical decision should be based on the entire examination, history and lab results and not on troponin alone in a CKD patient. Assess baseline labs if possible. Troponin can be elevated in patients with CKD in the absence of acute coronary syndrome, especially troponin T. There is no easy answer to this problem. Use your clinical judgement and keep the suspicion of CKD high until proved otherwise.
Sepsis
Sepsis results in an inflammatory response, releasing mediators that depress the myocardium. This depression may lead to increased membrane permeability, resulting in a leak of troponin. This damage is usually not due to necrosis and is reversible. In other instances, a troponin increase can result from increased oxygen demand on the myocardium in the setting of reduced oxygen supply that does lead to myocardial injury. Increased troponin in the setting of sepsis is associated with increased morbidity and mortality. Do not conclude that a positive troponin is acute coronary syndrome in a sepsis setting. Unless there is clear suggestion from other features that sepsis has triggered a plaque rupture type acute coronary syndrome (requires relevant chest discomfort or dynamic ST changes). A troponin leak in patients with sepsis is associated with an increase in morbidity and mortality.
Acute Non-Cardiac Critical Illness
Patients in the intensive care unit are by definition critically ill. These patients may be ventilated, on inotropic support, have a high core temperature, tachycardia, hyper- or hypotensive, and most likely are not healthy at baseline. All of this increased myocardial demand leads to a pathologic process. And in result, troponin elevation can be seen with increased cardiac demand (type II NSTEMI) and unfortunately is associated with higher morbidity and mortality rates. Do not conclude that patients with non-cardiac critical illness and elevated troponin without other manifestations of acute coronary syndrome (ACS) have had an acute myocardial infarction. ECG and history are vital. Troponin elevation in the critically ill has a correlation with mortality and morbidity. However, utilisation of ECG and history are important in differentiating demand ischemia and another cardiac event.
Amyloidosis
Amyloidosis is caused by a build-up of an abnormal protein called amyloid in organs and tissues throughout the body. The build-up of amyloid proteins (deposits) can make it difficult for the organs and tissues to work properly. Without treatment, this can lead to organ failure.
Rhabdomylosis with Myocyte Necrosis
It is important to emphasise that with rehydration, the initial treatment of rhabdomyolysis, troponin levels revert to normal. It is important at this stage not to subject the patient to either conventional or multidetector CT coronary angiography, to prevent contrast nephropathy. These patients could be reassessed for coronary artery disease after the episode of rhabdomyolysis with non-invasive imaging for significant ischemia and subsequent management determined accordingly.
Further Reading
- emDocs: The Elevated Troponin: What else besides ACS could cause troponin elevation?
- American Heart Association: Mahajan VS, Jarolim P. Clinician Update: How to Interpret Elevated Cardiac Troponin Levels. Circulation 2011;124:2350-2354.
- NCBI: Differential Diagnosis of Elevated Troponins
Peer reviewed by Elved Roberts, Malcolm Smith & Mark Williams