#SimBlog: Acute Upper GI Bleed #1
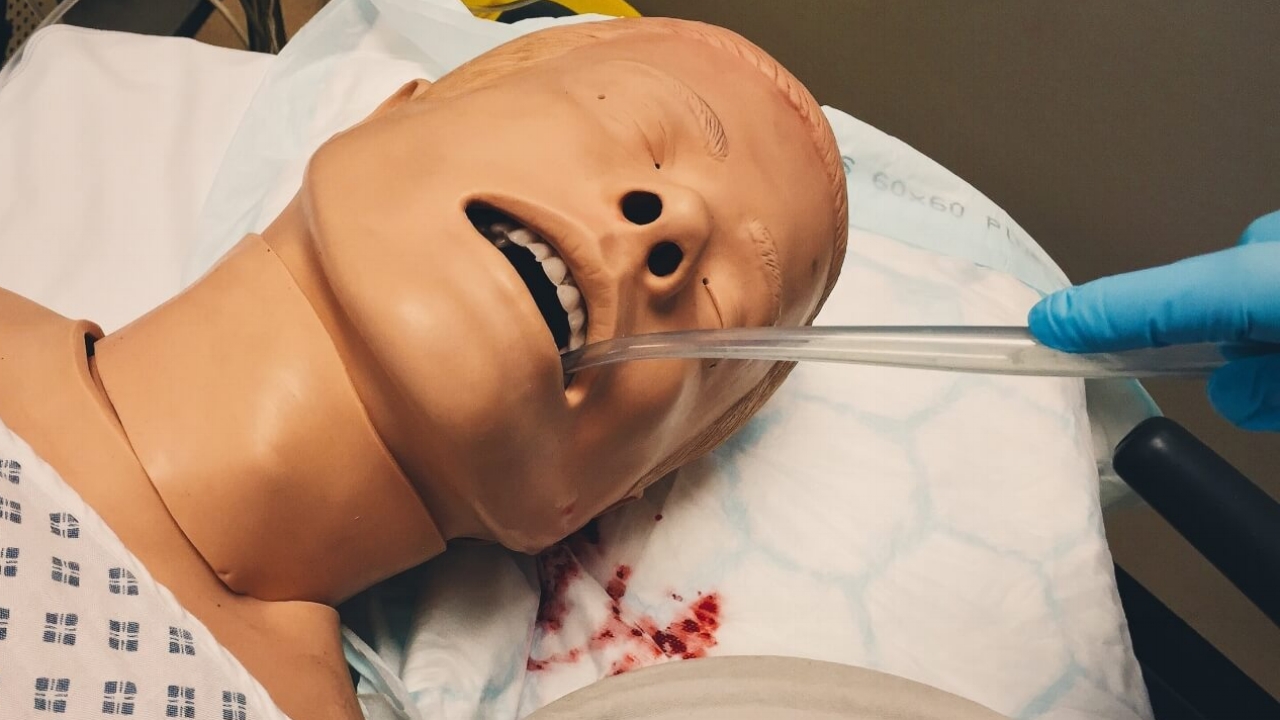
““A 61-year-old male is brought to the ER by paramedics with a history of 3 episodes of fresh haematemesis over the preceding 3 hours. No abdo pain or melaena.””
Observations
A – Clear & self maintaining.
B – Rate 25, SpO2 98%. Room air.
C – Pulse 130, BP 87/60.
D – E4 V5 M6 pupils equal
E – Temp 36.9°C
Clinical Findings
Cold, sweaty and pale
Fresh blood visible around mouth and lips
Why We Simulated?
Acute upper gastrointestinal bleeding is a common medical emergency that has a 10% hospital mortality rate. Despite changes in management, mortality has not significantly improved over the past 50 years.
Learning Points
Use local pro formas where available – they provide useful prompts when assessing severity and initiating treatment.
In patients presenting with upper GI bleeds consider recruitment to the Halt-It trial.
If a patient is bleeding and haemodynamically unstable despite appropriate resuscitation activate Massive Haemorrhage protocol.
Reference:
- NICE Guideline 141: Acute Upper Gastrointestinal Bleeding Management
Positive Feedback
Good preparation pre-arrival, clear allocation of roles within team
Recognised massive GI bleed and resuscitated with blood
Early institution of variceal bleed care bundle