#SimBlog: Major Haemorrhage
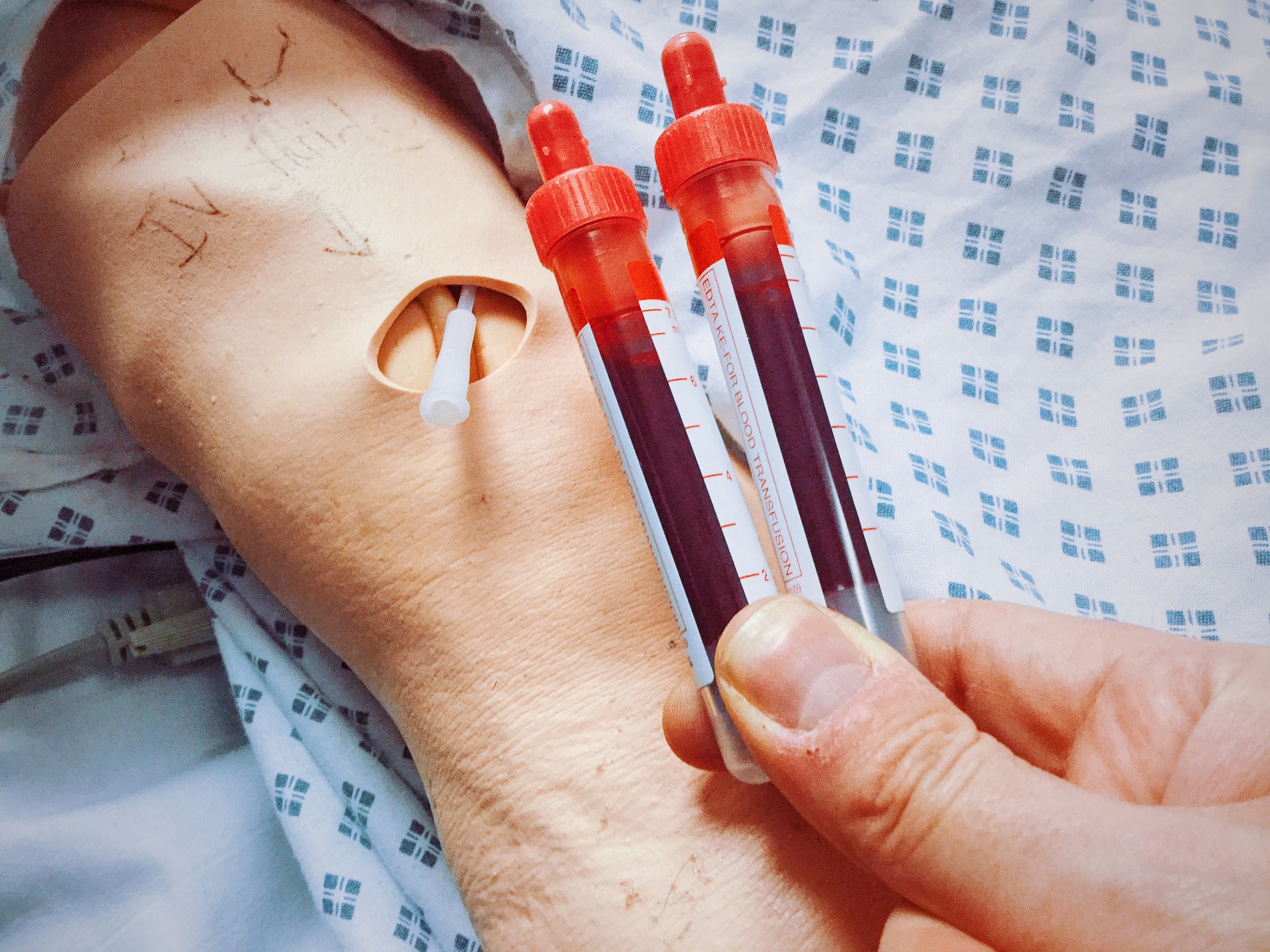
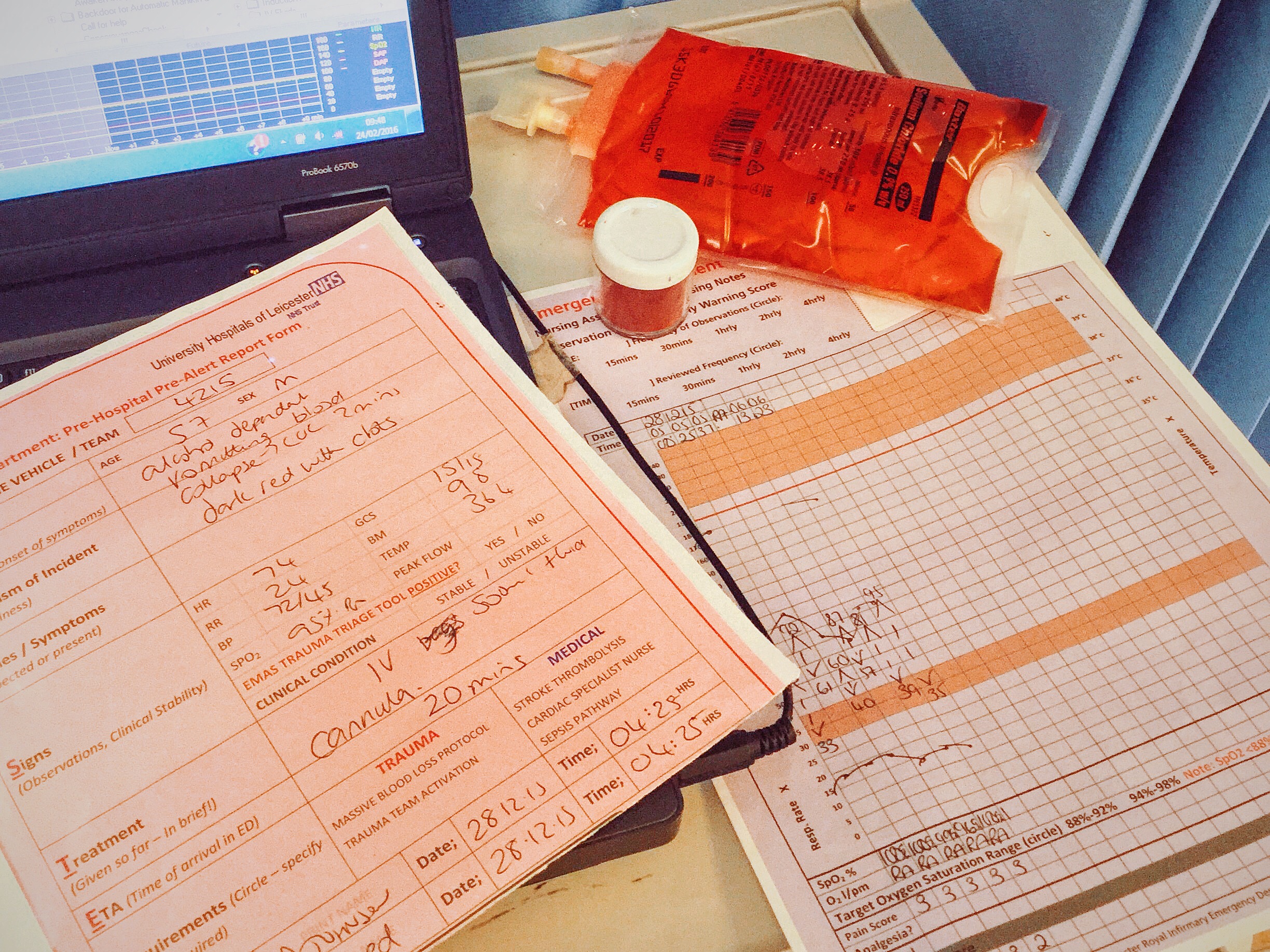
““57-year-old with collapse following an episode of haematemesis. Hypotensive pre-hospital despite 1500mls IV fluids.””
Observations
A – Patent, self-maintaining
B – RR 24, SpO2 95% in air
C – HR 74, BP 72/45
D – GCS 15/15
E – Temp 36.4°C, BM 9.8
Clinical findings
Lightheaded
Active fresh haematemesis
Pale
Why we simulated?
GI bleeding can result in considerable blood loss, it is important to consider the possibility of a variceal bleed (Fig. 1). Administering broad-spectrum antibiotics and terlipressin to these patients as part of the variceal care bundle can improve outcomes.
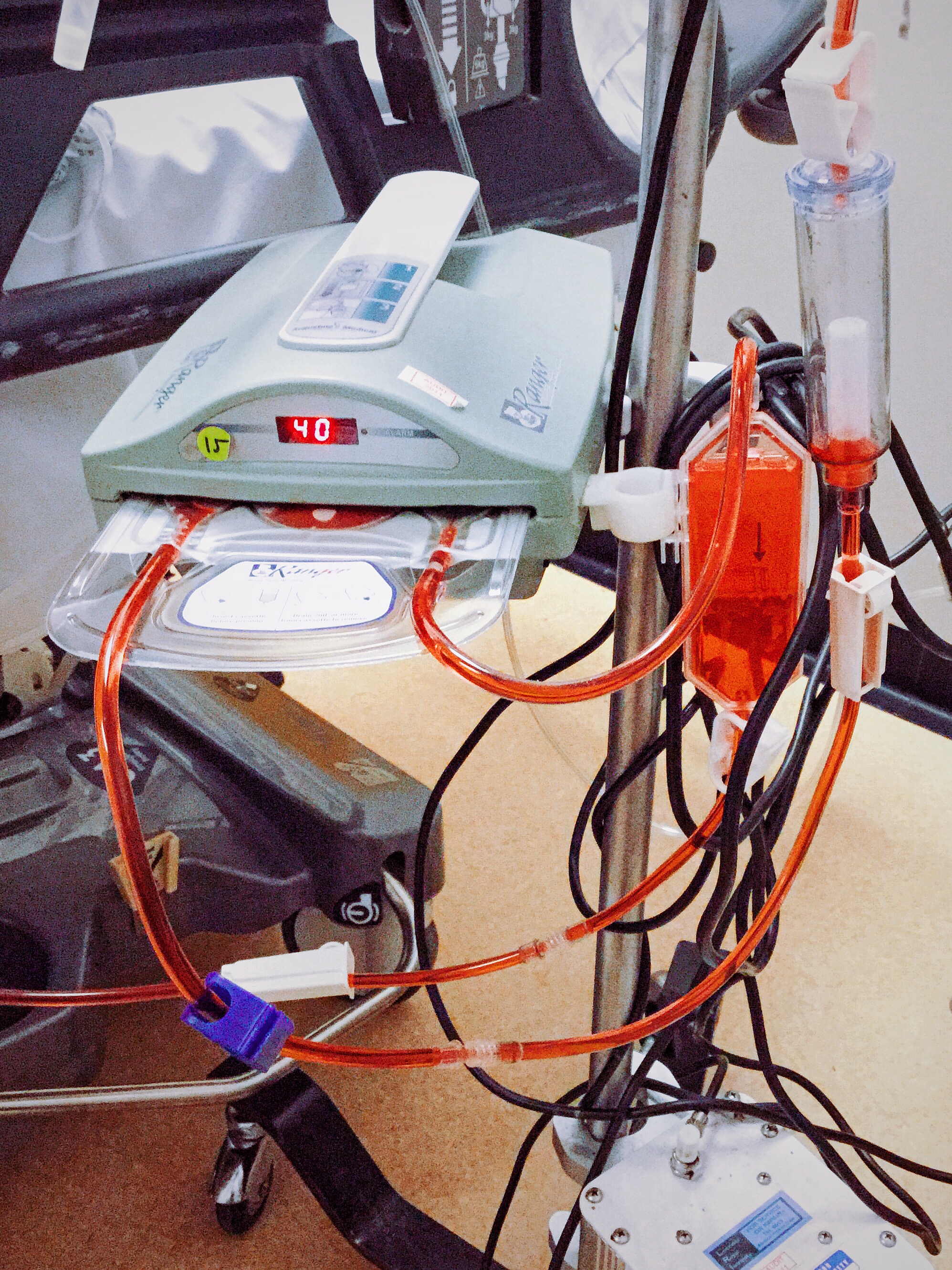
Definitive management will always be about "stopping the tap", however resuscitation may be required before or whilst this is happening. Transfusing only packed red cells can have consequences for the patient's coagulation.
In the case of massive blood loss or transfusion the Massive Haemorrhage Protocol (MHP) should be used. By activating your Massive Haemorrhage Protocol you will have access to large volumes of red cells quickly, but also to the other blood products your patient will need.
The Joint United Kingdom (UK) Blood Transfusion and Tissue Transplantation Services Professional Advisory Committee (JPAC) recommend running regular drills "to test the protocol and ensure the rapid delivery of all blood components"... So we did!
In conjunction with our colleagues in Transfusion Medicine we simulated a patient with a massive upper GI bleed and activated our Massive Haemorrhage Protocol... for real.
Further Reading:
- Lightning Learning: Major Haemorrhage
- NICE Guideline (CG141): Acute Upper GI Bleeding in over 16s
- #EM3 ACCS course: The Unconcious Patient, Haematemesis and Melaena
Learning Outcomes (ED)
In Leicester we activate the Massive Haemorrhage Protocol by dialling "2222" and informing switchboard that a Massive Haemorrhage is declared.
Consider administering tranexamic acid in patients with severe bleeding.
Remember to keep communicating with the patient.
Positive Feedback (ED)
Early administration of blood as resuscitation fluid.
Appropriate initiation of Massive Haemorrhage Protocol.
Good use of summarising throughout the scenario.
Learning Outcomes (Blood Transfusion)
When the MHP is activated lab staff should not be asking if cross matched components are required. Components should be issued according to MHP.
Lab staff should begin thawing AB FFP (or ABO compatible if valid sample available) as soon as Massive Haemorrhage declared.
Blood should have been available 15 mins from when the sample was received. in this instance the process took 25 mins.
Positive Feedback (Blood Transfusion)
Massive Haemorrhage paperwork was completed correctly.
Once the sample had been received communication with the clinical area was good.
Edit & Peer Review by Jamie Sillett & Rebecca Prest
Special thanks to the Blood Transfusion team for allowing us to run a "live fire" SIM with real blood, and to Jamie for literally bleeding for Simulation!