#SimBlog: Neutropenic Sepsis
WARNING: this post pre-dates SEPSIS 3.0 & may refer to older definitions
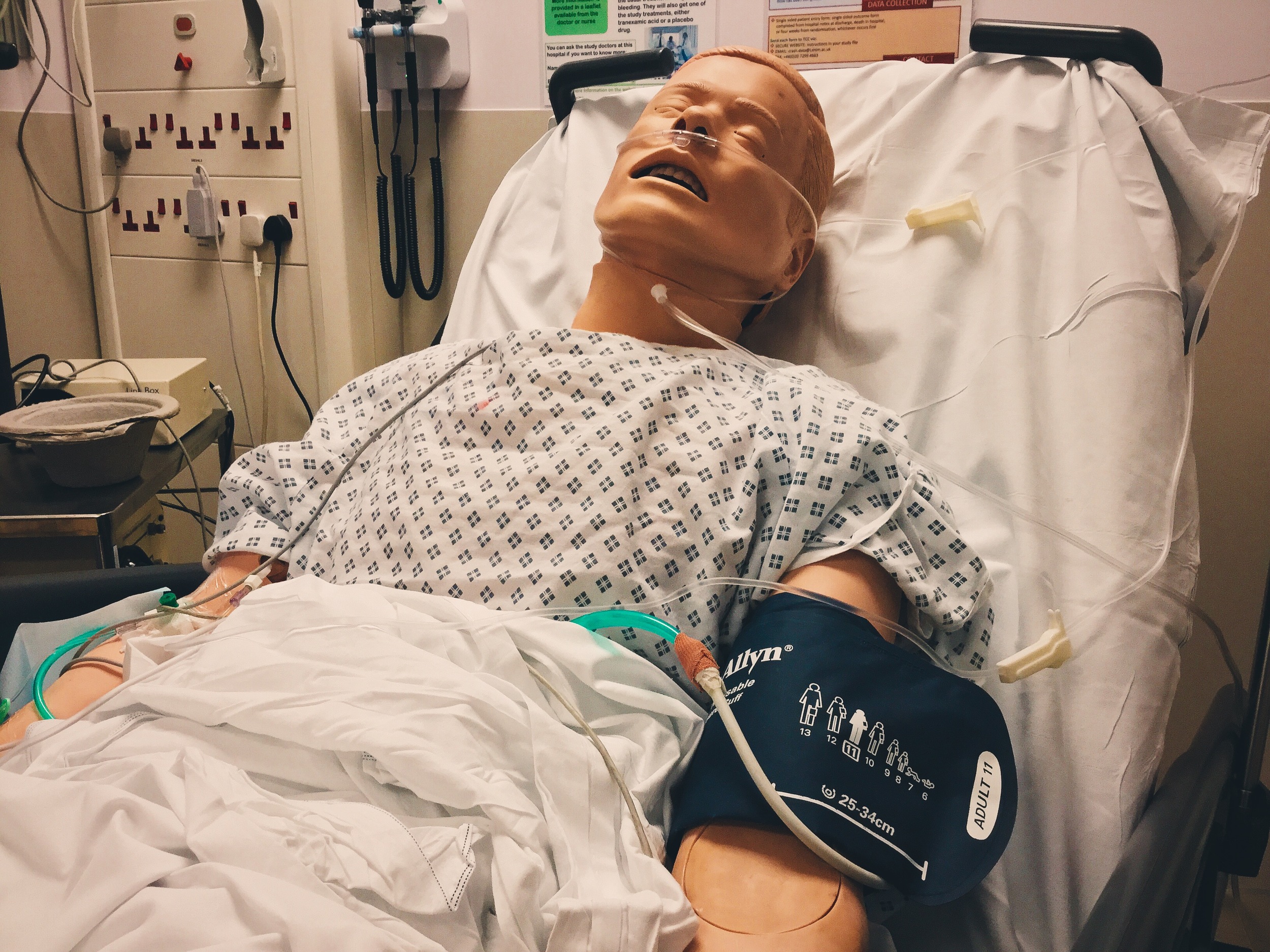
““53-year-old presented after an episode of collapse whilst trying to stand up from sofa. He had D&V for 2 days and hasn’t been eating or drinking well. He has received 1.5L saline by paramedics. He also has had abdominal pain for 1 day.””
Observations
A – Clear & self maintaining.
B – Rate 22, SpO2 100% on O2.
C – Pulse 110, BP 86/51.
D – E4 V5 M6,pupils equal
E – Temp 38.2°C
Clinical Findings
Creps at base of chest.
Generalised tender abdomen
Why we simulated?
This case is based on a real life patient, and unfortunately the outcome was poor - this resulted in an incident and subsequent investigation. By working through the case again we are able to highlight some of the areas of practice that could have been done differently.
Mortality rates for neutropenic have been reported to be as high as 21% (Nice 2012) so these patients are important to identify and treat early. Any patient who has recently had chemotherapy should be considered HIGH RISK for infections (don't forget the ED is often also full of sick people, so consider isolation and reverse barrier nursing to protect those with neutropenia).
Learning outcomes
Early Identification and treatment of Sepsis is crucial.
Nausea and Pain are important symptoms to control, but sometimes they will need to be left until the patient is more stable.
In patients with suspected neutropenic sepsis commence empiric antibiotics immediately – there is no need to wait for a neutrophil count. Our local antibiotic of choice is piperacillin with tazobactam (as per NICE guideline), give meropenem if penicillin-allergic.
When referring to specialties try to give concise opening line conveying your level of concern as well as the reason for referring.
Stopping to recap with the whole team will allow everybody to understand the management priorities and the next steps to be taken.
Positive feedback
Neutropenic sepsis suspected early.
Used local guideline to manage condition.
Good communication with patient throughout scenario.
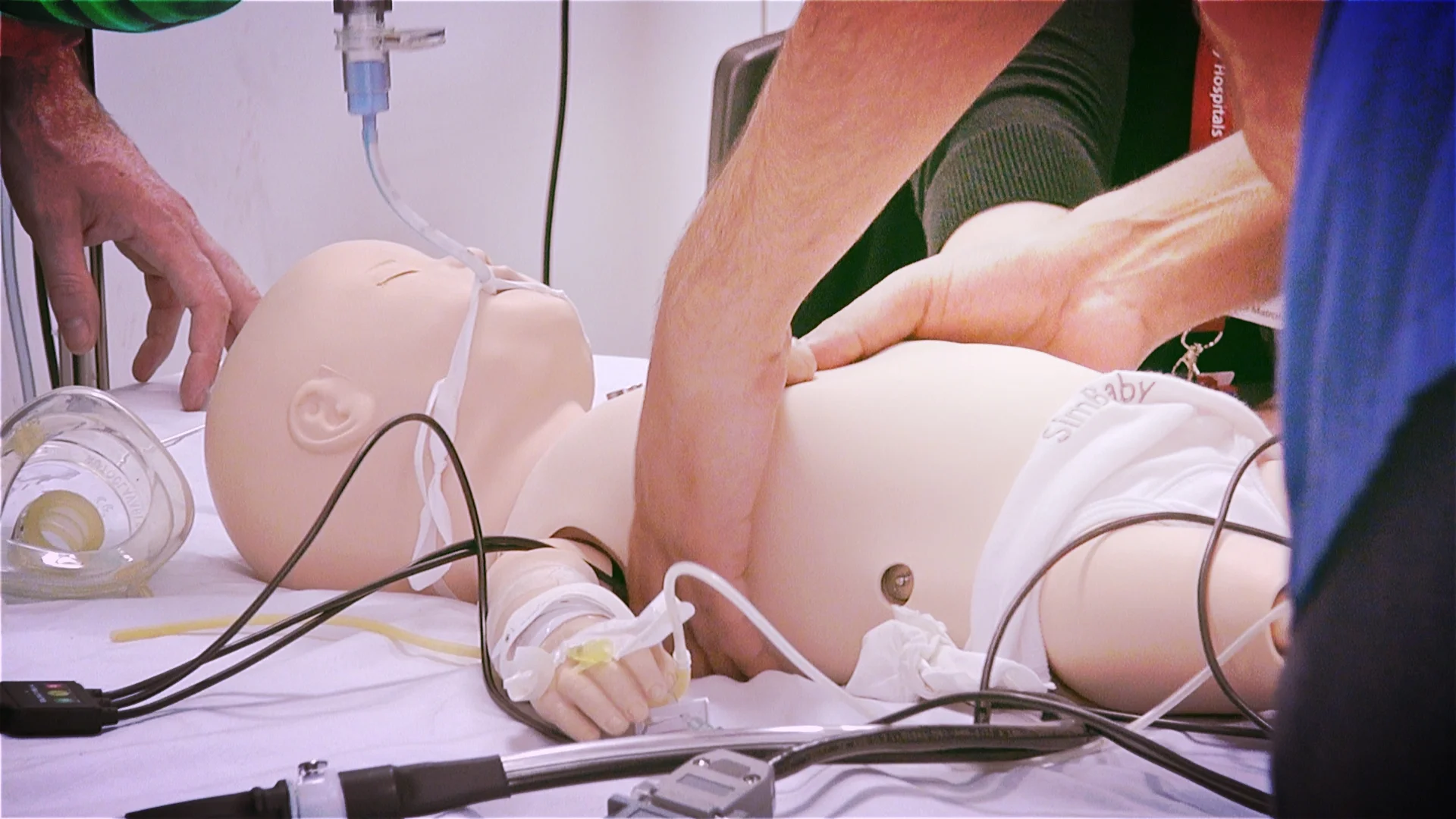
MDT simulation
Thank you once again to the haematology/oncology team who joined us for this simulation. Training with each other is a great way to put faces to the voices on the end of the telephone and is especially vital when we use simulation to cover cases generated via clinical governance.