Sim Blog: Acute Upper GI Bleed #2
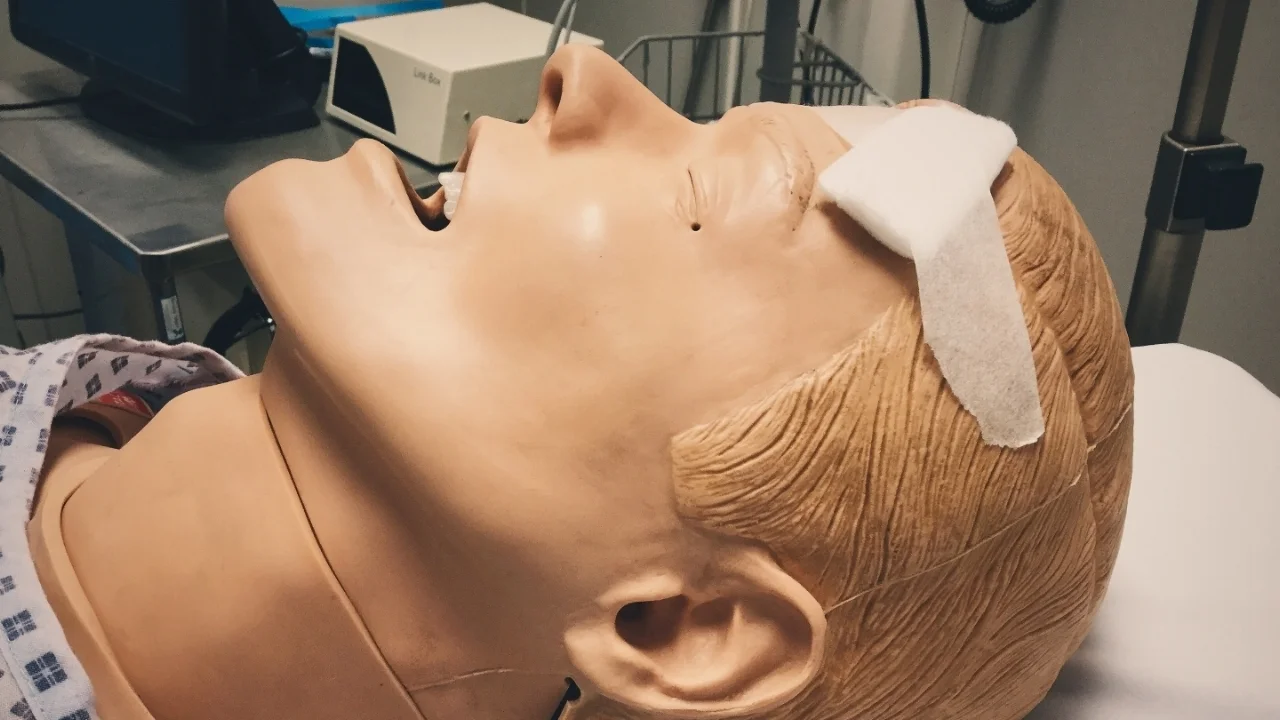
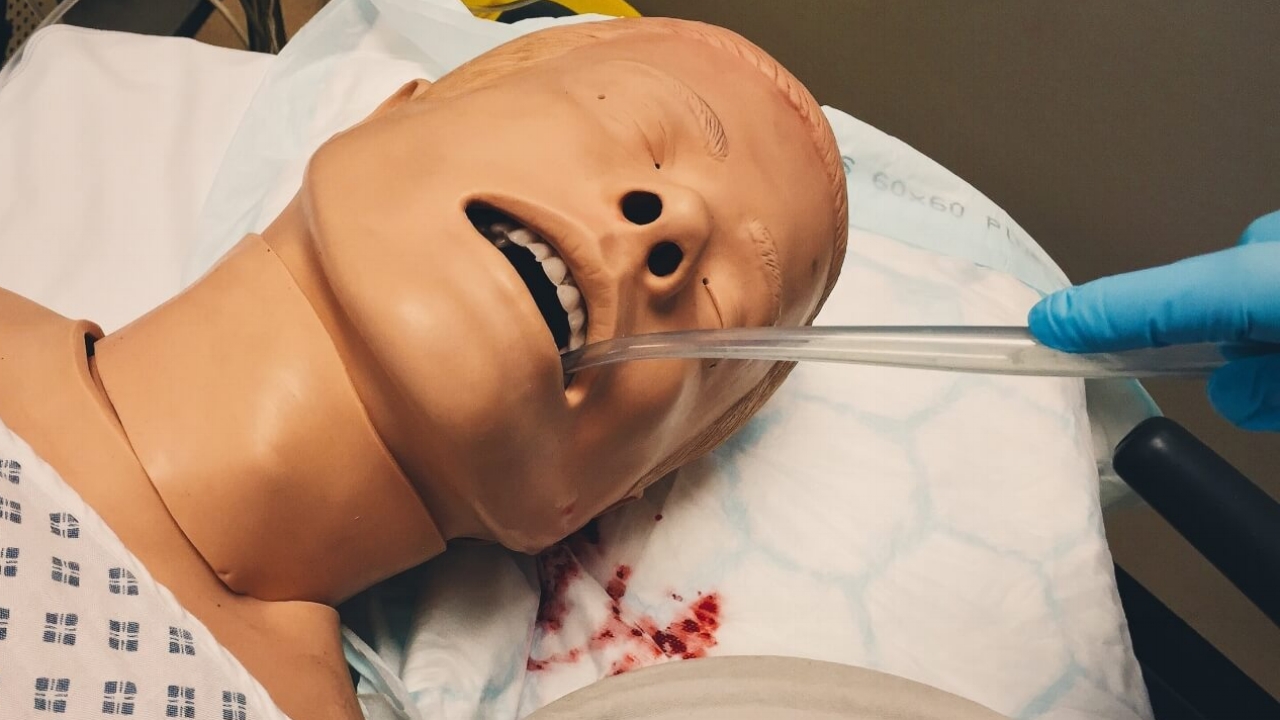
““A 51-year-old male is brought into the ER by paramedics with a history of fresh haematemesis over the preceding 3 hours. He has passed melaena and has some abdominal pain.””
Observations
A – Clear & self maintaining.
B – Rate 25, SpO2 98%. Room air.
C – Pulse 130, BP 87/60.
D – E4 V5 M6 pupils equal
E – Temp 36.9°C
Clinical Findings
Cold
Sweaty
Pale
Fresh blood visible around mouth and lips
Why We Simulated?
When managing the bleeding patient it is important to "stop the tap" and this is relevant to bleeding from any source.
However patients may also require resuscitation before they can be transferred for definitive management.
For large volume blood loss activating the major haemorrhage protocol will provide an adequate supply of blood products and alert all involved that the patient is critically unwell.
Learning Points
Remember that for large bleeds you should activate the Major Haemorrhage Protocol, this will ensure a supply of blood products will be made available.
It is important to pause and re-assess with the whole team to keep track of progress.
Treatments such as analgesia are important, but may not be the most immediate management priority in an unstable patient.
Beware possible side effects of any drugs you give, cyclizine can raise the Heart rate, IV morphine can lower the BP.
Positive Feedback
Roles allocated prior to patient arrival
AUGI Bleed Proforma Ready
Escalation of treatments from Crystalloid to O-ve blood progressed with patients deterioration
Possible variceal bleed identified and treated
Good communications and team work from nursing staff