Racing Hearts: a case of paediatric SVT
““A concerned mother rushes to the emergency department with her 12-month-old child who has had symptoms of a URTI, a one-day history of poor feeding and a single episode of vomiting.””
Why did we simulate?
Supraventricular tachycardia is the most common rhythm disturbance encountered in paediatric patients, composing over 90% of arrhythmias in children therefore, most clinicians will encounter this at least once at some point in their careers [1]. In children, SVT usually occurs due to atrioventricular re-entry (AVRT), including Wolf-Parkinson white syndrome. Early recognition of adverse features(shock, syncope, myocardial ischaemia, heart failure) is critical in SVT as it will guide the management of the arrhythmia [2]. Hence, an efficient ABCDE assessment is essential when initially presented with such patients, as well as a good understanding of resuscitation guidelines [3] and early senior input.
Observations
Systolic BP = 82
Pulse = 220
Saturations = 95% (on air)
Temp = 37.2
RR = 50
Initial Clinical Findings
A – Alert, strong cry
B – Equal air entry bilaterally, no crackles or wheeze, mild retractions, mild nasal flaring
C – CRT of 2 seconds centrally and peripherally, normal femoral pulses, no cyanosis, pink in colour
D – BM: 5.5, GCS 15, PEARL 3mm
E – No rashes, abdomen SNT, no organomegaly, no bruising, no evidence of bleeding, Temp 37.2°C
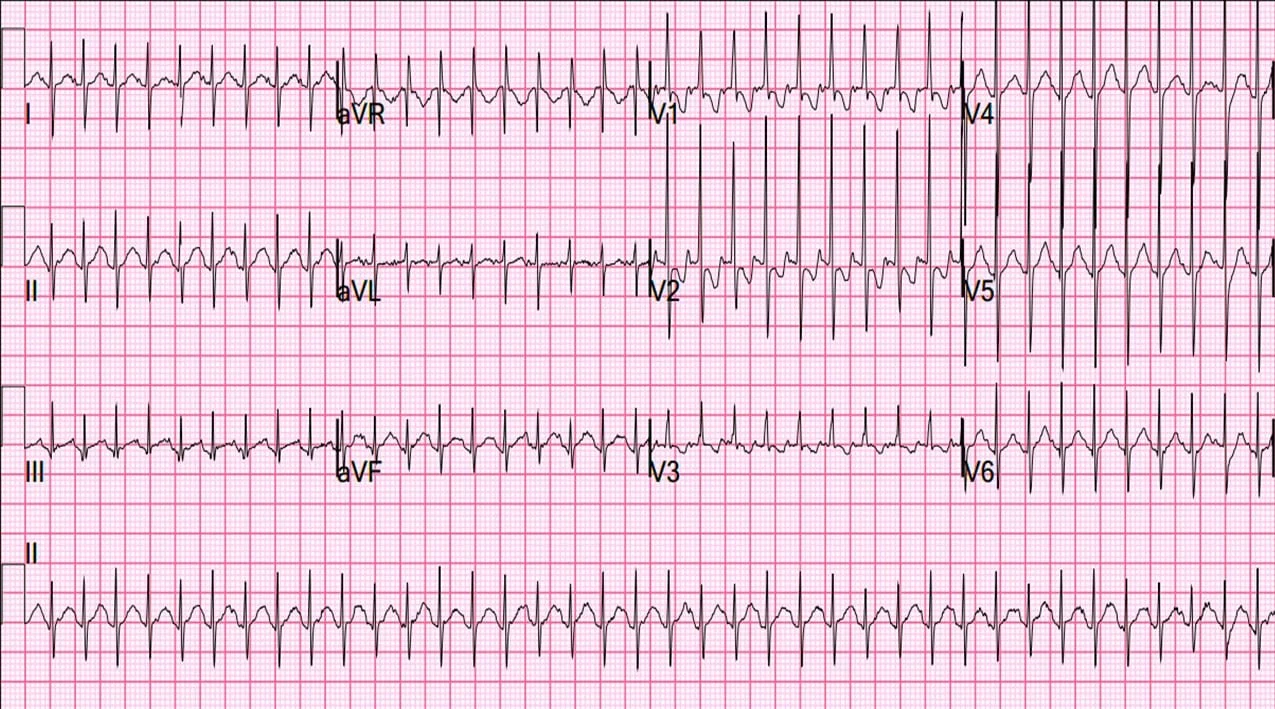
Initial ECG
Simulation outcome
The team realised the patient was in a stable SVT rhythm, with no response to either vagal manoeuvres or adenosine. The patient then progressed to having an unstable SVT and the team performed a synchronised cardioversion.
ECG post-cardioversion
Learning Outcomes
Vasovagal manoeuvres
These can be more difficult in young children if they are not able to correctly follow instructions and will be dependent on the age of the child.
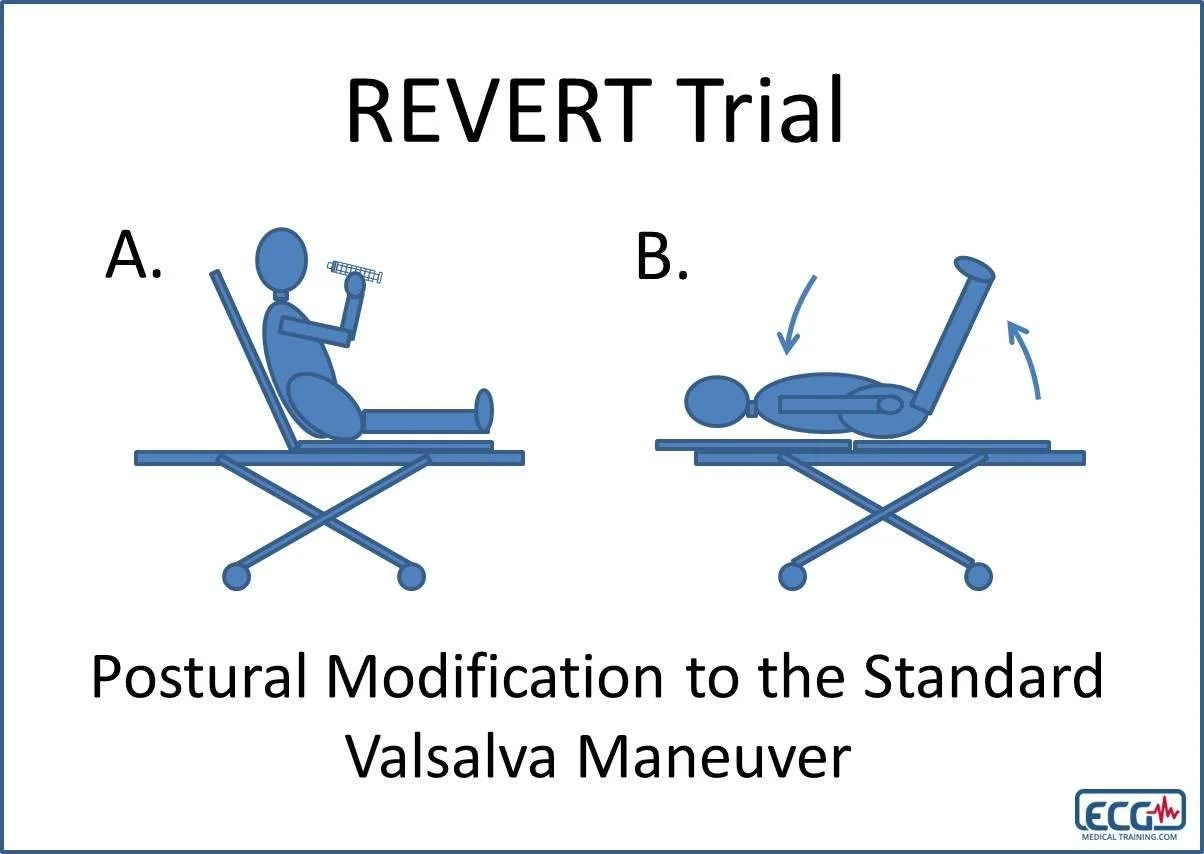
Modified Valsalva: Increasing the thoracic pressure by blowing on a 10ml syringe for 15 seconds with the patient in the semi-recumbent position, followed by supine repositioning with 15 seconds of passive leg raise at a 45-degree angle. [4]
Other options for less cooperative patients include direct application of ice to the face or asking children to bear down.
Check out this video by The Lancet for a demonstration of the modified Valsalva manoeuvre…
Situational awareness: Managing paediatric SVT requires situational awareness and the ability to anticipate potential deterioration. Team members should be alert to changes in the patient's condition and anticipate the potential need for escalation of care.
Teamwork and role clarity: In a high-stress situation like paediatric SVT, it's crucial to have well-defined roles and responsibilities. Teams should establish clear expectations and protocols for managing paediatric SVT to ensure that everyone knows their role and can work together effectively.
Parental communication: it is of course expected for parents and relatives to be emotional and concerned for their child, naturally you want to do everything you can to make sure the relatives feel involved and understand what is happening. However, in these time-pressure situations, it can be difficult to balance the care of the patient with communication with relatives.
Staff feedback
“Great experience simulating working effectively in time-critical scenarios with unstable patients.”
“Found it useful practising how to adapt the management approach to changes in the patient’s condition.”
Advice for educators going forward:
Following our experiences with this simulation, we highlighted the following as potential areas of improvement…
Smaller groups reflect the reality of the workplace: It was suggested in post-sim feedback that too many participants and spectators were distracting and it was suggested that in future sim scenarios that it should be more akin to true clinical practice.
Earlier escalation for help: Escalating to the senior members of the team should be done early as soon as the acuity of the situation has been realised in order to guide the simulators on the right course of management.
Modify scenario and/or intensity based on the level of the learners: This simulation can be tailored based on the experience of the learners. This can range from a simple stable SVT appropriate for medical students to a more advanced scenario involving the management of deteriorating patients and the use of advanced life support techniques.
Peer reviewed by Dr Sunny Jutla