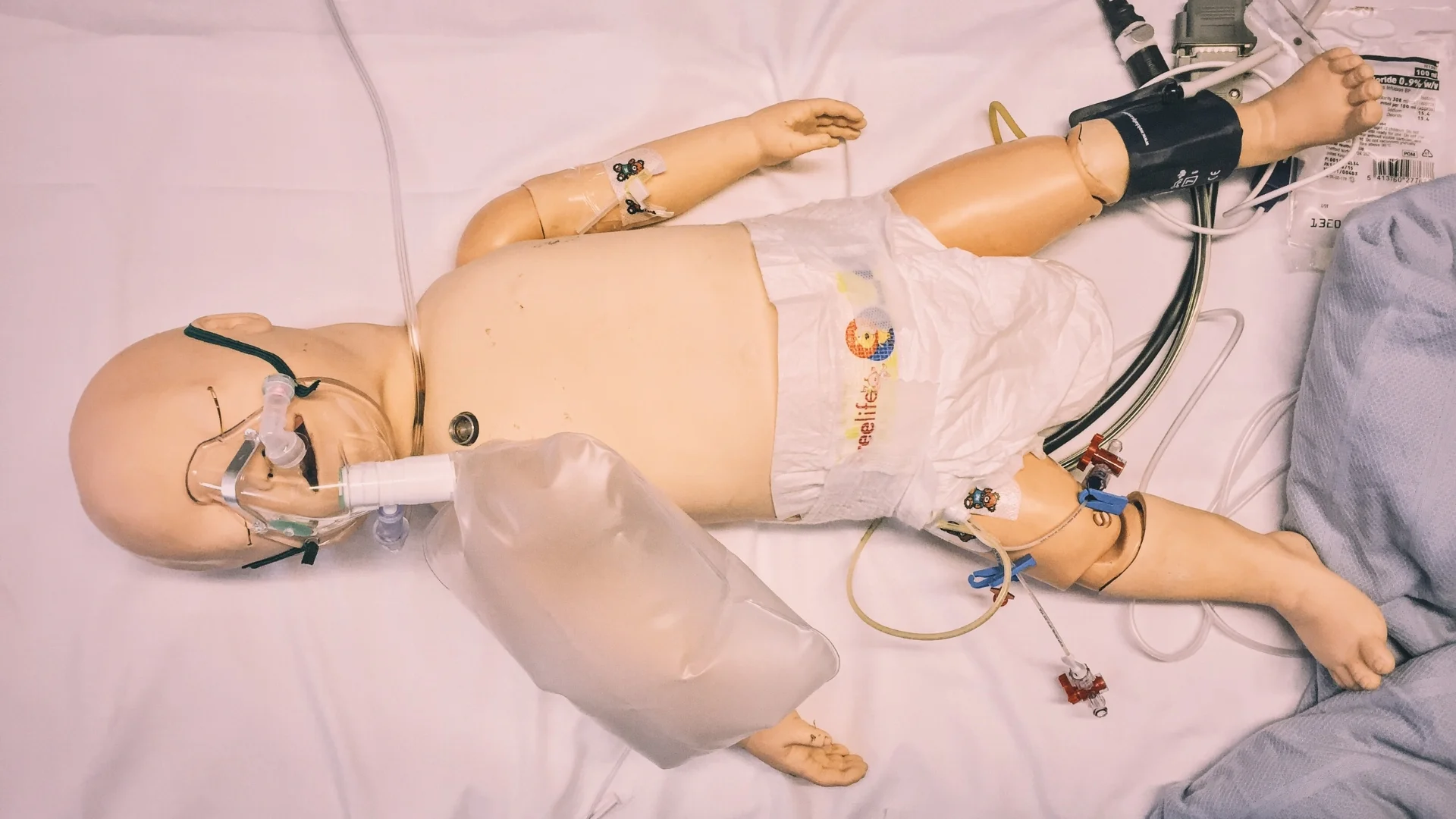
#SimBlog: Does He Need A Bolus?
““You review a 2-year-old with a 7-day history of fever. Today he has stopped eating and drinking.””
Observations
A – Patent
B – RR 40, Sats 97% in air, mild recessions
C – HR 180, CRT 2 seconds, BP 100/50
D – GCS 15/15, BM 4
E – Temp 39.5°C
Clinical Findings
Dry lips
Spleen felt at 4cm below ribs
Healing mosquito bites over abdomen
Small amount of urine in the nappy
Gas: Lactate within normal range, Hb 70
Why We Simulated?
In the ED, we see many feverish children with deranged observations. Our triage system assigns a Paediatric Observation Priority Score (POPS) to the child, which is used within priority grading. In this simulated case, the child ultimately had an underlying diagnosis of malaria. The emerging learning themes for this scenario were:
Assigning and Interpreting a POPS
Our patient scored 6 on his POPS, with a breakdown of:
Recessions: 1
Raised respiratory rate: 1
Tachycardia: 2
Temperature: 1
Gut feeling: 1
(low-level concern)
We wanted our staff in the ED to be able to recognise that this score in combination with the present clinical signs is suggestive of someone who is sick. A score of 4 or more on our POPS also indicates the need to complete our Paediatric Sepsis Screening Tool. This example shows how to work through our tool, which in this case led to the identification of Red Flag Sepsis and initiation of the Paediatric Sepsis 6. Follow the link here to watch our Sepsis Screening Guide.
Distinguishing Between Shock and Dehydration Clinically
This patient presented with a 1-day history of poor oral intake and drier than usual nappies in the context of a fever for the last 7 days. Cardiovascular examination revealed a tachycardia with dry lips, normal skin turgor, a central CRT of 2 seconds and a blood pressure within a normal range for age. There was a small amount of urine in the nappy. Blood gas revealed a normal lactate.
Children with clinical signs of shock should receive a fluid bolus to help restore their circulating volume followed by careful reassessment and early consideration of inotropic therapy. However, often the temptation in the sick but ‘not shocked’ patient is also to prescribe a bolus of fluid. The difficulty in the latter situation comes when there is little clinical change following the bolus and therefore you face the conundrum of whether this is because the child remains intravascularly deplete or whether the bolus was not warranted in the first instance.
We wanted our team to understand that the findings in this scenario were suggestive of clinical dehydration, rather than decompensated shock and know how to prescribe IV fluid therapy accordingly.
This information is summarised in the infographic below. Please see the NICE Guideline for Algorithms for IV Fluid Therapy in Children and Young People in Hospital for more information.
Are boluses beneficial? The FEAST Trial
The Fluid Expansion As Supportive Therapy (FEAST) trial was a landmark study investigating the effects of fluid boluses in the resuscitation of febrile children in Africa with evidence of poor perfusion. The trial studied children (ages: 60 days to 12 years) with shock, and analysed whether there was a mortality difference between resuscitation with bolus fluids compared to the use of maintenance fluids only. Results showed maintenance fluids conferred a 3.3% survival benefit over either bolus of albumin or saline. The mortality at 48 hours was 7.3% for those who were given no bolus, versus 10.5% for either fluid bolus [1].
Whilst there are notable differences when comparing this population to our own, including a high incidence of anaemia and malaria amongst those included in the study and a lack of intensive care, it does emphasise the importance of careful assessment with regard to fluid resuscitation.
References:
- Life in the Fast Lane : FEAST and Paediatric Fluid Resuscitation
Further Reading:
- #EM3: The Returned Traveller
- UHL Childrens Medical Guideline: Management of Malaria in Children
- Centers for Disease Control and Prevention: Fever in the Returned Traveller
Learning Outcomes
A POPS of 4 or more warrants completion of a Paediatric Sepsis Screening Tool.
Discussion as above regarding the difference between shock and dehydration and the appropriate fluid management for each.
If the response to treatment is not as you expected, re-evaluate your management plan and discuss the case with a senior.
Positive Feedback
Focused history taking revealed recent travel.
Maintained broad differential, treating for bacterial sepsis even though there was a high suspicion of malaria.
Good vocalisation of thought process by team leader throughout scenario.