#SimBlog: Severe Sepsis
WARNING: this post pre-dates SEPSIS 3.0 & may refer to older definitions
““A 79-year-old man from a nursing home found unresponsive by staff this morning. Off his food yesterday.””
Physiology
A – Clear & self-maintaining
B – Rate 25, SpO2 94% in room air
C – Pulse 120, BP 91/65
D – E4 V4 M5, pupils equal
E – Temp 38.9°C
Clinical Findings
Dehydration ++
Chest clear
Abdomen soft
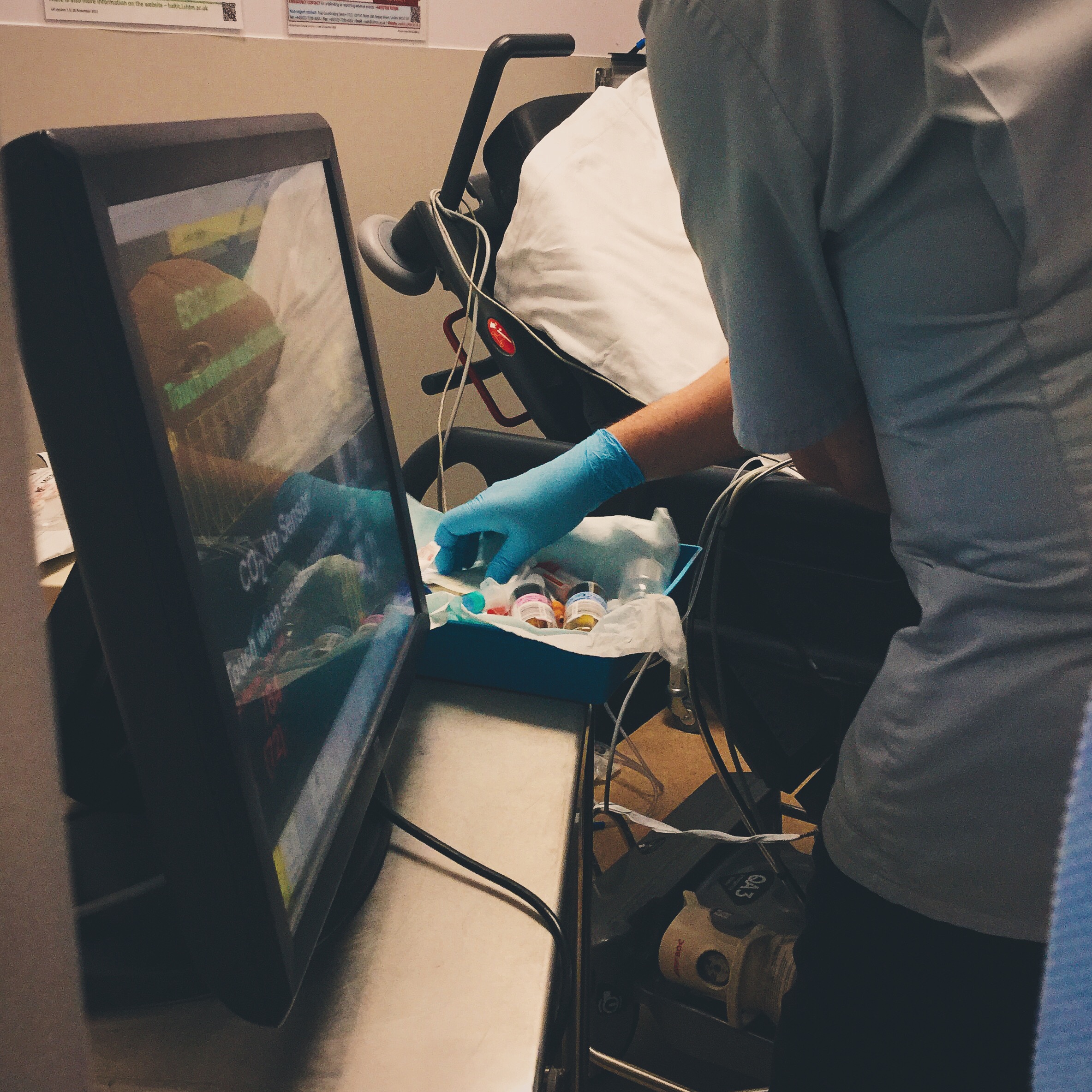
Why We Simulated
Sepsis is a condition we see very commonly within the ED and this is an illness in which timely management in our department can make a significant difference to the patients outcome.
We know that sepsis is often poorly recognised and treated. For the most unwell patients every 1 hour delay in the administration of antibiotics results in an 8% increase in mortality.
References:
-
Sepsis Trust – http://sepsistrust.org
Learning Points
Using our Sepsis pro forma can help aid timely management and decision making for patients.
Reassessing regularly helps ensure situational awareness and allows an opportunity to check nothing has been missed.
Try to ensure that you speak directly to a particular person rather than asking “somebody” to do it and “close the loop” on all communication. These strategies can help avoid situations where everybody thinks someone else has done a particular task, which can delay treatment for patients.
Positive Feedback
Suspicion of sepsis identified and management plan communicated pre-arrival.
Early fluid administration.
Recognition that patient not improving and senior help sought.