#SimBlog: I Just Got A Needlestick!
““Whilst suturing a wound on an unconscious patient’s head I caught my thumb with the needle...””
Observations
A – Patent
B – Normal
C – Normal
D – Normal
E – Small wound to thumb of right hand
Clinical Findings
No other injuries
Broken glove and skin
Why We Simulated?
The exact incidence of sharps injuries is unknown (there is likely to be a degree of under reporting), A review by J. C. Trim and T. S. J. Elliott found a mean rate of 4.0% (range 1.0±6.2%) sharps injuries per 10,000 healthcare workers.
Healthcare workers in the ED and in other areas are all at risk of these injuries and they are likely to present to the ED, especially out of hours.
Definitions
A sharps or 'needlestick' injury is: "breakage of the skin barrier by a potentially contaminated sharp."
A splash injury is: "exposure of broken skin or mucous membrane to a body fluid."
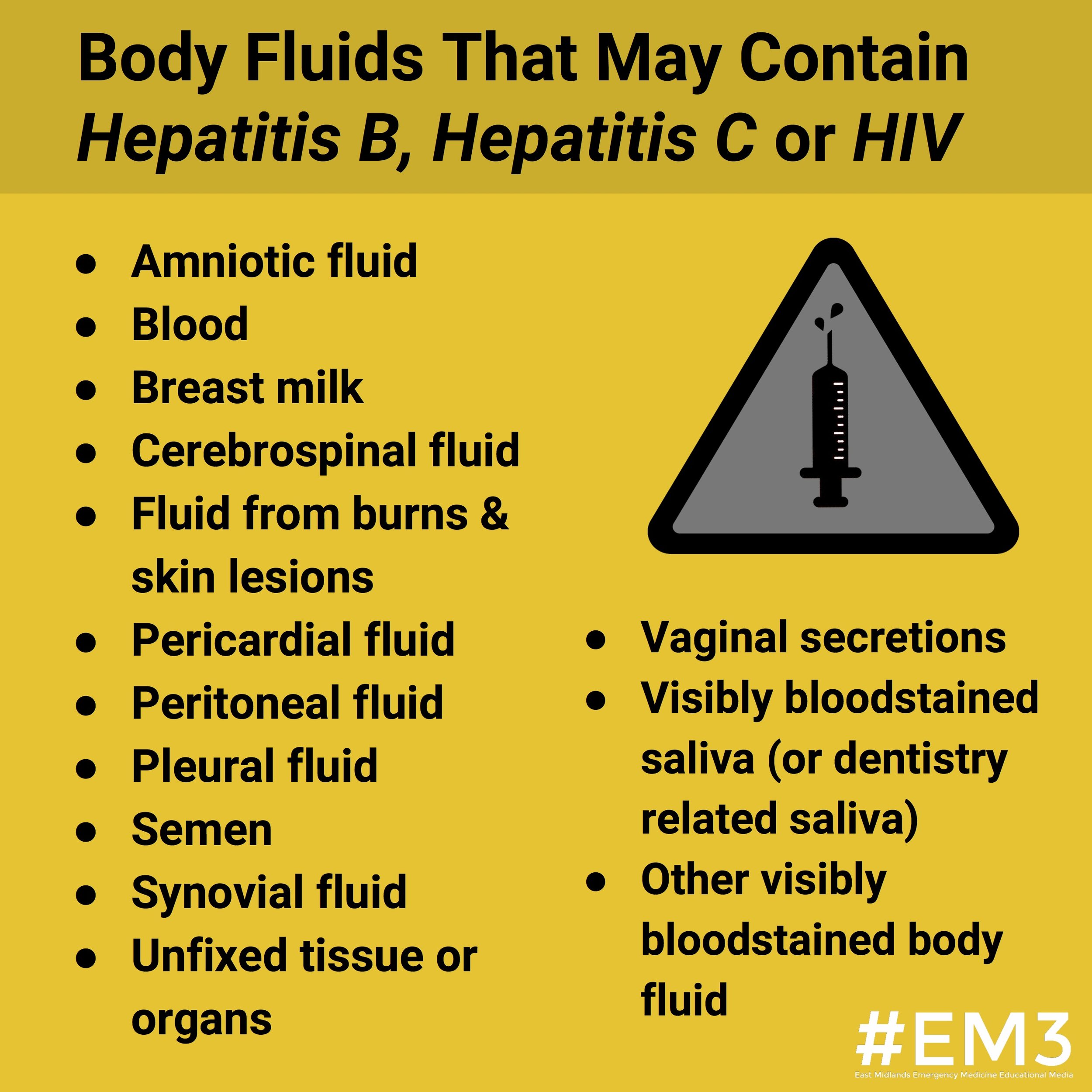
Significant exposure is defined as:
"Percutaneous...exposure to blood or body fluid from a source known to be, HBV surface antigen (HBsAg), HCV, or HIV positive."
Saliva, urine, vomit and faeces are all considered to be low risk fluids.
Clinical assessment and risk stratification
Assessment of risk should consider the incident risk and the source patient, it will involve a number of factors from the history and your examination.
Incident Risk: can be categorised as minimal, low or high risk as follows:
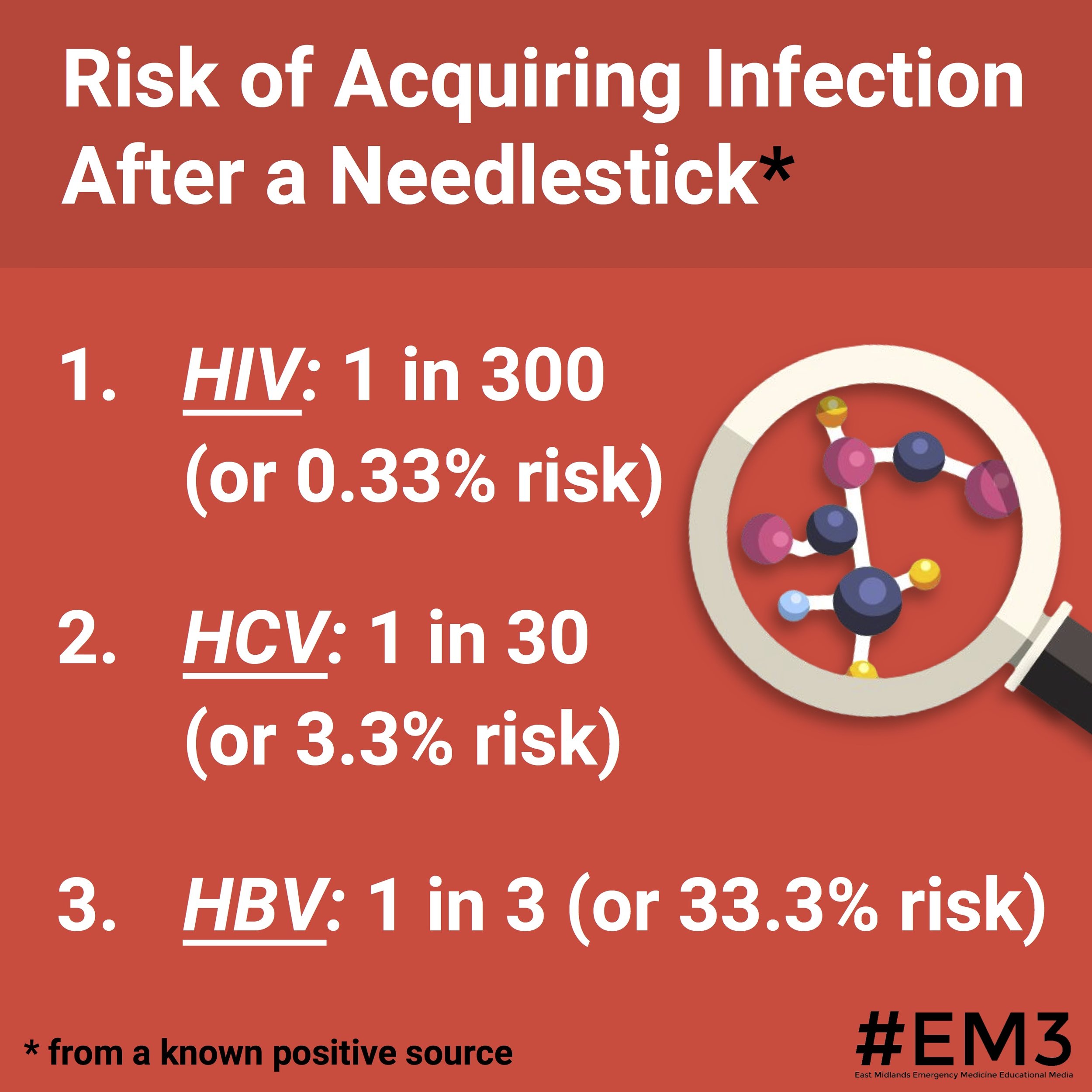
Source Risk: the risk assessment of the source patient should begin with whether they are known to have one or more blood borne virus.
For those known to have a BBV:
If the viral load or treatment status is unknown then it should be regarded as a High Risk exposure
Patients with detectable viral loads or untreated/advanced infection should also be regarded as high risk
Only patients who have an undetectable viral load or have good adherence to long term treatment should be regarded as low risk
If they are not known have a blood borne disease then further risk assessment should be made, including the presence of risk factors and any recent negative test results.
Management
This will be altered by the risk assessment you have made and local policy, however the key points are summarised below. Our local policy is available through the hospital intranet.
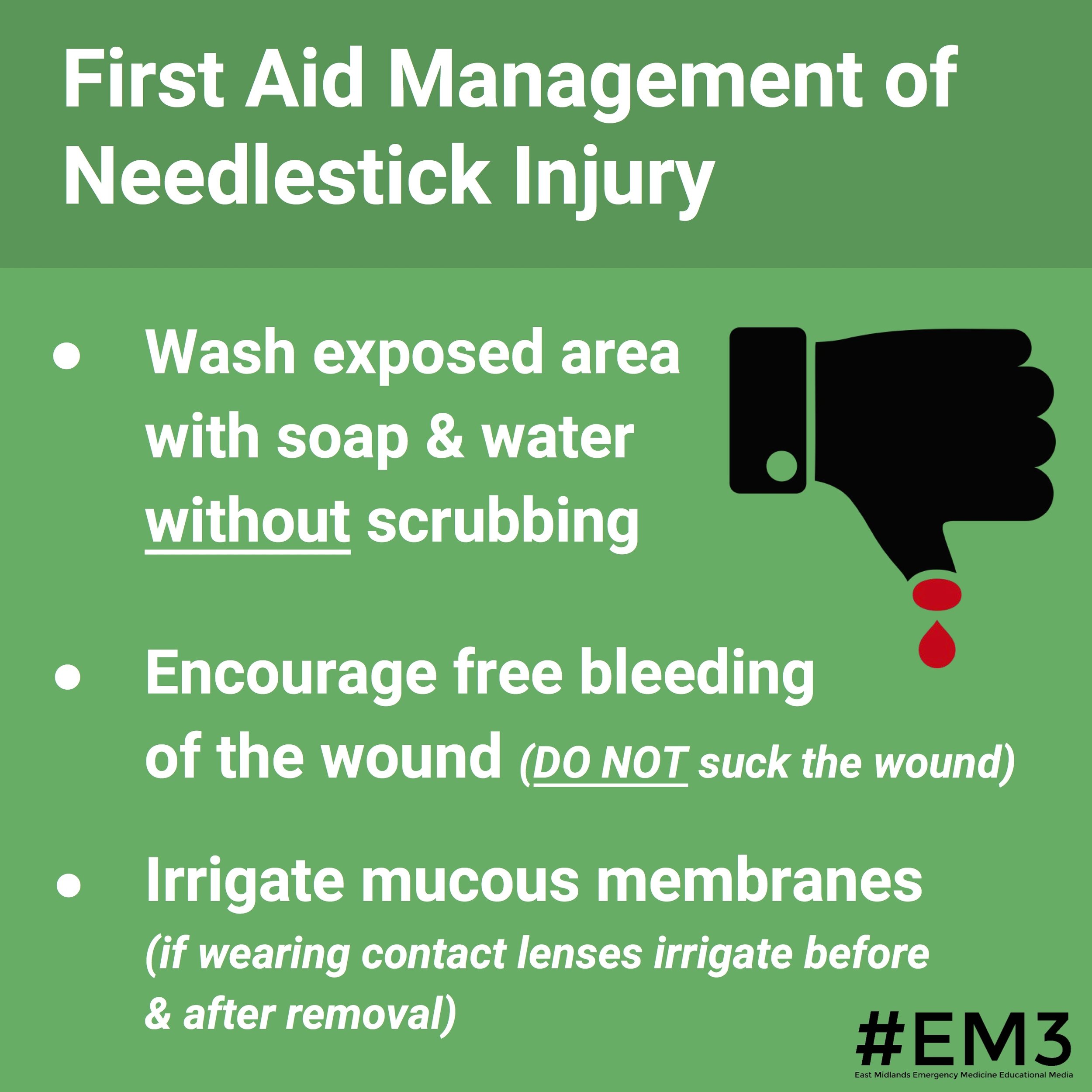
First Aid:
Wash the exposed area with soap and water without scrubbing
Encourage free bleeding of the wounds (DO NOT suck the wound)
Irrigate mucous membranes (if wearing contact lenses irrigate before and after their removal
Recipient:
Serum Save for BBV testing
Ensure has had HEP B vaccine. They may need a booster or accelerated course +/- HBV immunoglobulin
Post-Exposure Prophylaxis (PEP) is available for HIV and this should be started if recommended by local policy
There is no post-exposure treatment for HEP C
Occupational health should be informed
Should be advised re: barrier contraception and blood donation
Source Patient:
Management should not be by the recipient of the exposure
Inform them of what happened
Council them that it is standard practice to screen for BBV with their consent
You should be prepared for how you will manage them if they do test positive for any BBVs
Our case is complicated by the fact the patient is unconscious and unable to consent. Current UK law does not allow you test for HIV when the patient cannot consent unless it is in the patient's interests to do so. There is an excellent summary of the issues this raises here.
Further Resources:
Learning Objectives
Remember to follow the departmental protocol
Follow the correct procedure for incident reporting
Understand that you will need to disclose what has happened to the donor patient
Positive Feedback
Stopped our simulated doctor from sucking the wound as part of first aid
Recognised need to risk assess source patient
Considered the legal and ethical aspects of an HIV test on an unconscious patient