#SimBlog: End of Life
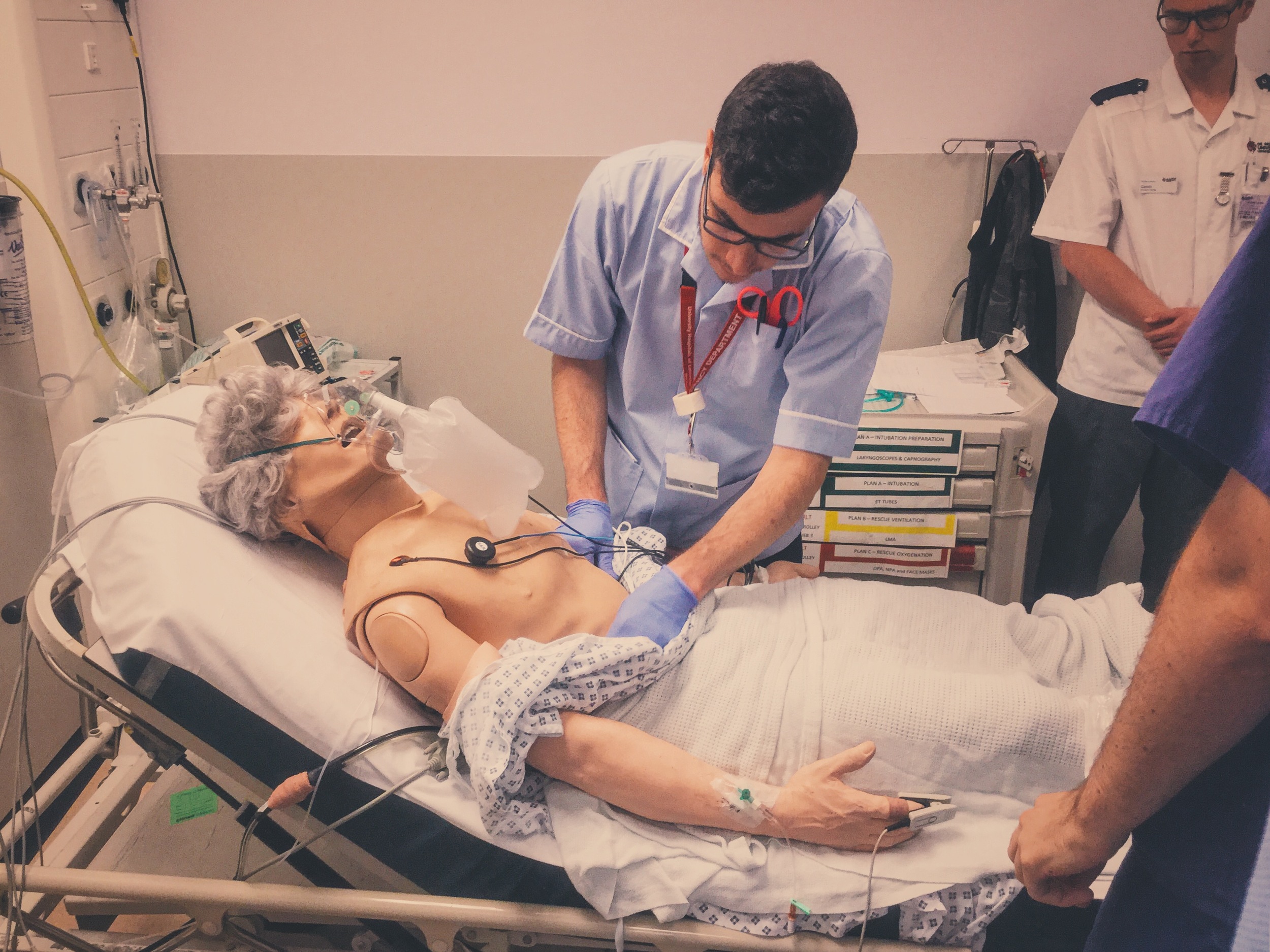
““87 year old from a nursing home, found unresponsive this morning. Recent discharge from community hospital after #NOF and Pneumonia.””
Observations
A – Patent
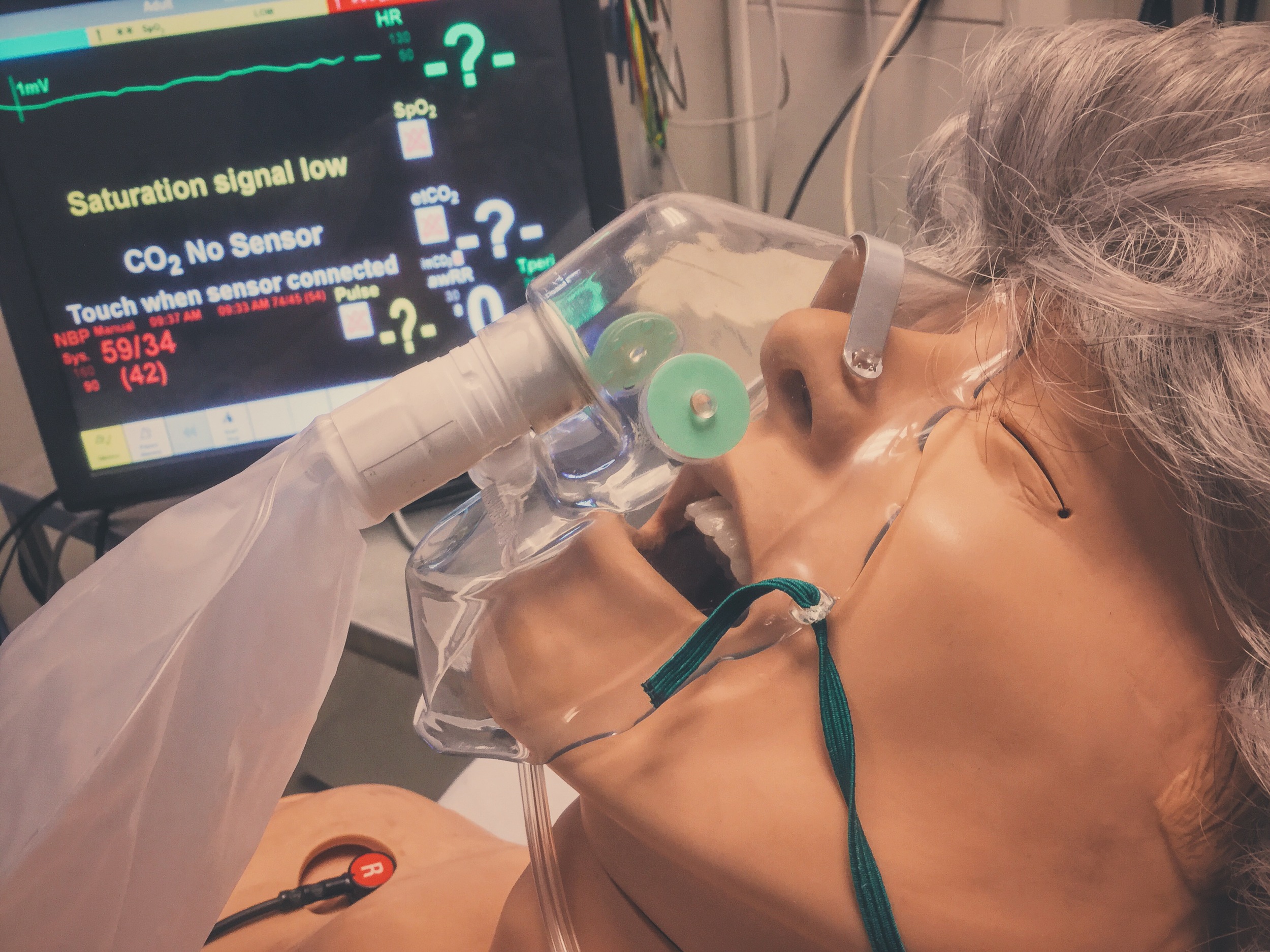
B – Bilat Air Ent, Sats 88%, RR 12
C – HR 40, BP 87/56
D – GCS E1 V2 M1
E – Temp 35.6°C
Clinical Findings
All observations deteriorating over the next 15 minutes
Why We Simulated?
End of Life care matters. We will all die and the circumstances of how will often be remembered by families and relatives. More than this there is a patient at the centre of it all who may be distressed, scared or in pain. It falls to all of us to give our patients the best death we can.
There are those who believe the ED is not the best place to die (and for some patients they are right). Ideally decisions should be made in advance and death can be in at home or in a hospice, but some deaths are not expected or planned for.
We need to be able to recognise a patient who is dying and address the needs of the patient and their family. We need to remain sensitive and considerate to their views, and there are sometimes hard conversations to be had such as resuscitation status.
There is also benefit in recognising the patient who is not dying imminently but who is deteriorating over time. It may not be the best role for the ED clinician to try and address this fully, but we can plant a seed with the patient or their family that thought needs to be put into how future deterioration is managed.
This blog can't tell you the right way to approach end of life care, but there are some useful resources to help guide you (see below). Management should include treatment for pain, distress, nausea and respiratory secretions and there are standard treatments for these.
I also would like to steal some thoughts from a recent Listening in Action event held at our trust and ask you to consider what is it like when a patients dies or is dying in your department:
For the patient?
For the family?
For the staff?
Finally what can you do to make things better for all three groups?
Further Reading:
Learning Outcomes
Recognition of the dying patient can be challenging, consider some clues: physiology, co-morbities and recent admissions.
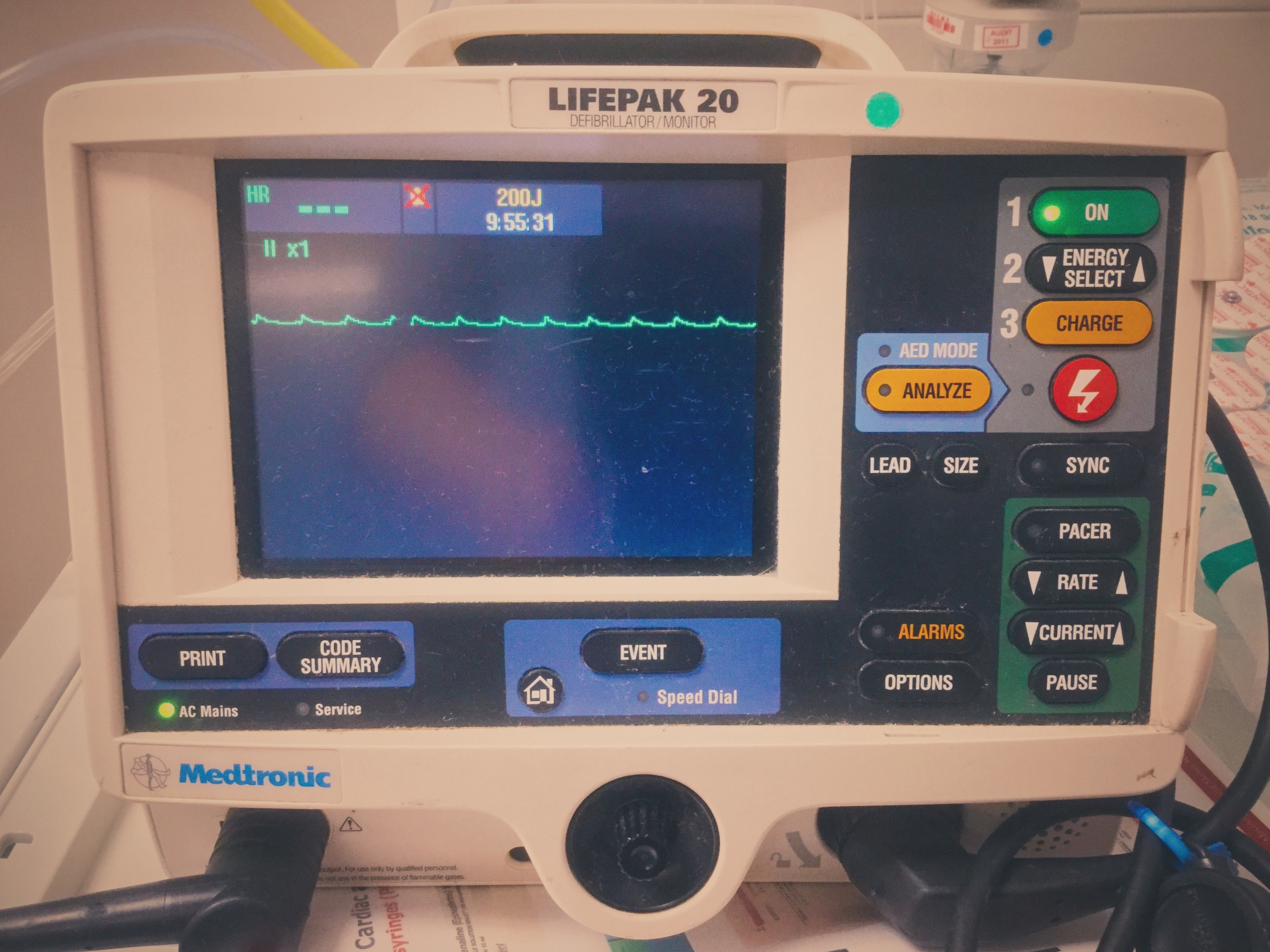
Less can be more – you do not always need to start resuscitation.
Glycopyrolate may be an appropriate treatment for bradycardia, but in an emergency atropine and adrenaline are readily available and familiar…
Positive Feedback
Sought senior advice to help with decision of escalation.
Recognised critically unwell patient.
Pre-allocation of roles.