The End of Life Care Jigsaw
“In this world nothing can be said to be certain, except death and taxes”
We have previously looked at some of the aspects of End of ife (EoL) care in our #SimBlog and again as part of our #GEMcon16 conference. However, it remains an important issue for those working in the ED and as has been said before you only get one chance to get End of Life care right!
I have recently changed hospitals as part of my higher specialist training and was able to attend a teaching session on End of Life Care in the ED at Northampton General Hospital.
This session was based on the concept of an End of Life Jigsaw and I would like to share this with you as I found it a really useful concept.
It is also worth addressing some of the aspects of the jigsaw for patients who are not actively dying but are at risk of further deterioration or death from their current illness.
To try and cover all aspects of the jigsaw in detail as one post would not do justice to the amount of work that has gone into this project, so this will serve as an introduction and we will expand on some sections in further posts.
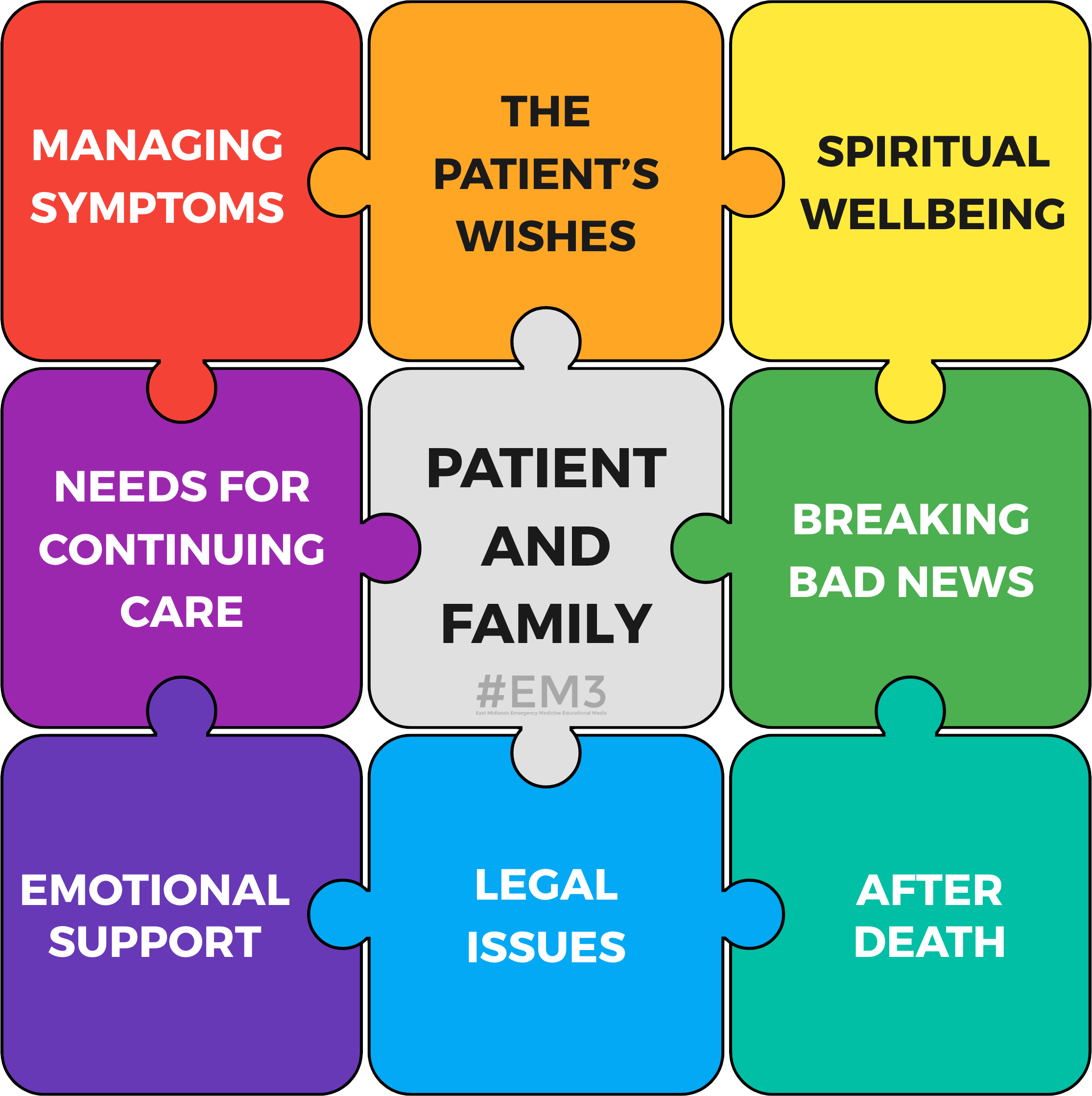
The Jigsaw
Most doctors when asked about EoL care highlight symptom management as their focus.
Whilst this is very important the jigsaw is designed to remind the clinician that the other facets of EoL Care hold equal weight, and therefore equal sized jigsaw pieces.
All pieces must also be considered and addressed to complete the picture and provide holistic care. It is worth noting to that some aspects of the jigsaw are relevant for patients with an uncertain prognosis, who are not actively dying but are at risk of further deterioration or death.
The Patient and Their Family
In the centre of the jigsaw is the patient as they are the centre of the ongoing care. It is worth considering that the patient's family can include others identified by the patient as being important to them, such as close friends.
Rather than asking "Is there any family you would like us to contact?" consider " Is there anyone you would like us to contact?"
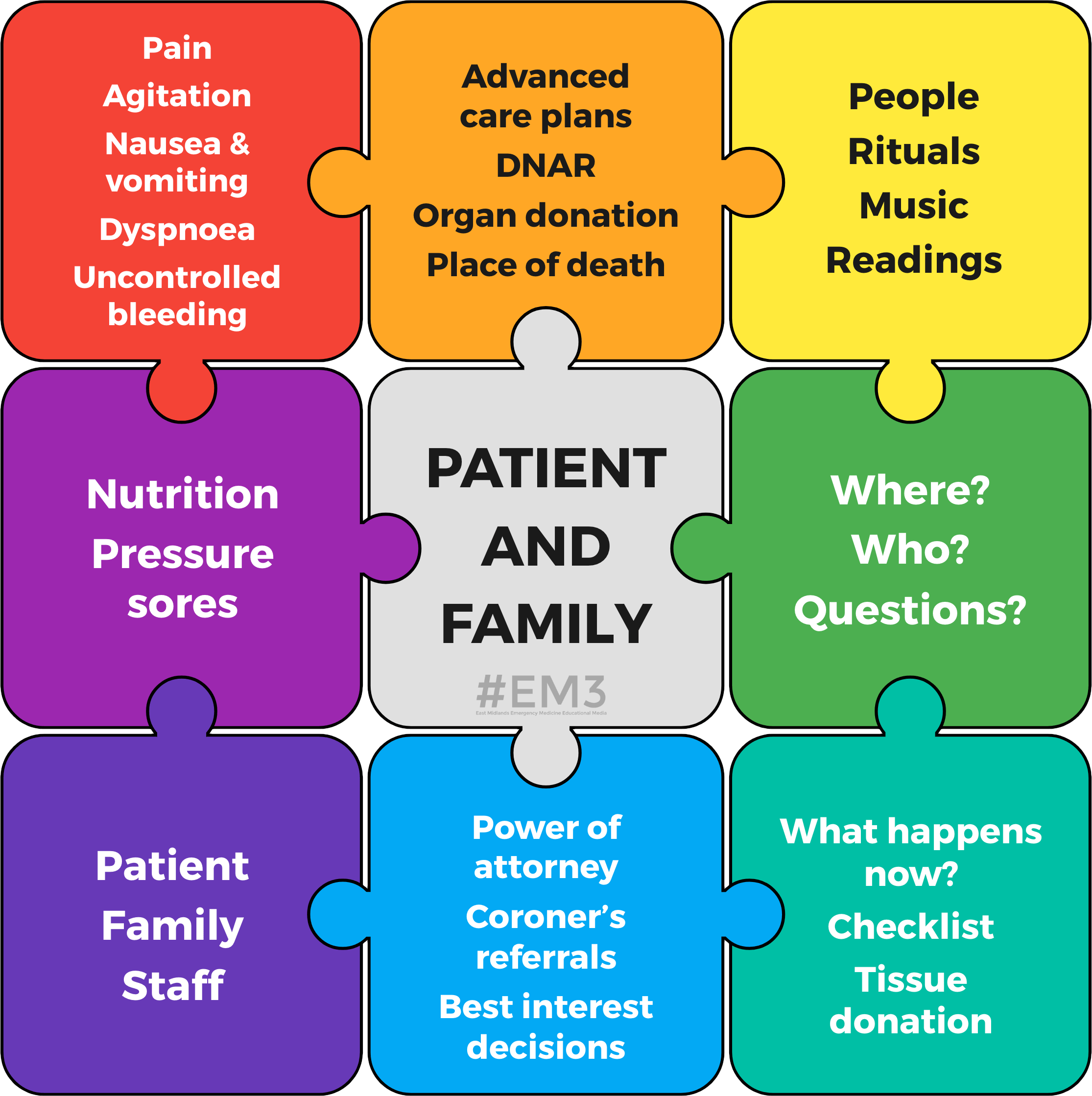
The Patient's Wishes
Consideration should be given to any advanced care plans, resuscitation status orders, organ donation as well as a preferred place of care. These discussions can be challenging and we have more on this in our ACCS Module.
Symptom Management
This should include:
Pain
Agitation
Nausea and vomiting
Breathlessness and Respiratory Secretions
Uncontrolled Blood Loss
The drugs and non-pharmacological interventions available for these symptoms are fairly well standardised and you should be guided by your local protocols. One of the thing that also came out of the teaching session was the use of dark (black) towels for those with uncontrolled bleeding as opposed to hospital issue white ones.
Spiritual Wellbeing
This can be easy to overlook, especially if like myself you don't follow a particular faith. However, asking "Do you have a faith that helps you in a time like this?" can be a good way of opening up the conversation.
Different faiths will have different practices and a working knowledge of common practices can be developed with experience, however, most hospitals will have on-call chaplaincy teams that may be able to help even for faiths not practiced by the chaplain themselves.
Continuing Care Needs
This may include mouth care, hydration and nutrition or pressure area care. There is also some overlap with symptom control here.
Breaking Bad News
Breaking bad news is a core skill for the Emergency Physician and just like practical skills such as chest drains it is one that is improved with study, practice and feedback. There is more on this available in our ACCS module on Breaking Bad News.
Emotional Support
It is important to consider support for the family and this is often provided by details given in bereavement packs.
However it is also important to consider:
Support for patients with no family
Debriefing and support for staff. This is more obvious when a case has been traumatic, but we also need to look out for staff members affected by other cases. For example was this a junior member of staff's first patient death, or are there similarities with a something happening in a staff members home life?
Legal Issues
Did you know that power of attorney can cover either financial matters or health and welfare? It is worth clarifying which (if any) is in place and ideally seeing any documents if possible.
For patients who no longer have capacity to make decisions for themselves and do not have an appointed LPA it may be necessary to make a "best interests decision" about their future care. Guidance for this is laid out in the Mental Capacity Act 2005. When this is the case it is important to involve the senior team.
Do you know which deaths require referral to the Coroner's Office? A brief overview can be found here.
After Death
What happens next? As a doctor I have found that this is not often covered by us nor do we receive a great deal of teaching on it. Every hospital will provide written information for bereaved families; I suggest that you find this booklet in your own department and have a look at the local procedures so you are better armed should you get questions from relatives.
Tissue Donation may be possible for patients even when organ donation is not, you can find more information from the NHS Blood and Transplant Service.
After Death Checklists are used in some departments to ensure all appropriate processes and paperwork have been completed, again it is worth having some knowledge of what they include.
Hopefully you have found this introduction to the jigsaw a useful starting point for the management of end of life care. We'd love to hear any feedback you might have or examples of good practice you use locally. Please get in touch via the comments below or social media.
Edit & Peer Review by Dr Sarah Vince
The End of Life Jigsaw and original teaching session are the work of Dr Sarah Vince, EM Consultant at NGH.